Impacting Children’s Physical and Mental Health through Kinesiology Support in Clinical Care: A Randomized Controlled Trial Protocol
Article information
Abstract
Objectives
To enhance the confidence of children and adolescents with medical conditions and disabilities to engage in healthy, active lifestyles. Children with medical conditions and disabilities often exhibit more sedentary lifestyles relative to peers and are at increased risk of poor health outcomes. Clinical experience suggests physical activity confidence is an important factor influencing physical activity participation.
Methods
This randomized controlled trial evaluates an evidence-based intervention targeting physical activity confidence among children and adolescents with medical conditions and disabilities. Potential participants, 8 to 18 years of age diagnosed with a medical condition or disability, will be screened for adequate physical activity motivation but a lack confidence. Consenting participants (n=128) will be randomized 1:1 to a 12-week in-person or virtual physical activity intervention (24 hours/week total) led by a Registered Kinesiologist or control (assessments only). The intervention will combine physical activity participation with education about physical activity knowledge, goal setting, motivation and self-management. Primary outcomes are self-reported physical activity confidence and motivation at baseline, post-intervention and three months following intervention completion. A secondary outcome will be daily physical activity minutes assessed by accelerometry. A repeated measures mixed model will be used to compare outcomes between the in-person intervention, virtual intervention, and control groups (alpha=0.05).
Conclusions
This trial aims to assess the impact of a novel application of behaviour change theory on physical activity confidence among children and adolescents living with medical conditions or disabilities. Increased physical activity confidence, knowledge and skills could enable these youth to lead a more active lifestyle.
INTRODUCTION
Despite a majority (>70%) of Canadian children knowing the physical activity guidelines for a healthy lifestyle [1], only one third engage in the recommended behaviour [2]. Even more strikingly, more than 90% of children with medical conditions and disabilities do not achieve the recommended levels of physical activity for optimal health [3,4]. This has significant quality of life [5] and health-related implications, with an increased risk for all-cause and cardiovascular disease related mortality [6]. Intervening to support physically active lifestyles early in life is particularly important given that physical activity declines during adolescence and adulthood [7].
In youth with physical disabilities, perceived competence, physical functioning, and mastery have been found to be significant correlates of physical activity [8]. Children with certain medical conditions can be hesitant to partake in physical activity due to fear of pain or exacerbating symptoms of their condition [9,10]. At the most fundamental level, individual behaviour is influenced by both intrinsic (within the individual) and extrinsic (other people or the individual’s environment) factors. Children with medical conditions and disabilities often lack confidence in their ability to successfully participate even when they are motivated to take part in physical activity [11–13]. The preparation stage of behaviour change [14] is for individuals who have decided they want to make a change and are in the process of planning how that will occur. These children and youth require support to develop a realistic plan that enables them to successfully move forward. As such, focusing on ways to set appropriate goals and develop a realistic action plan will build confidence around physical activity to help them transition from the preparation stage of behaviour change to the action stage [14].
Kinesiology interventions among children with medical conditions and disabilities have focused on how exercise or motor skill training can be used to improve physical activity and fitness [15–19]. A number of studies have looked at the benefits of physical activity interventions in children living with a cardiac diagnosis, chronic pain, physical disabilities, and/or concussion [15–17,20–22]. A limitation to these studies was that the focus on improving skills (e.g., increasing activity capacity) did not intentionally address other salient domains of behaviour change (e.g., confidence and self-efficacy, goal-setting, perception about ability to participate in physical activity) [19]. Factors such as self-efficacy, the use of mobility aids, and social support for exercise have all been highlighted as being important elements of physical activity interventions that are often not addressed through interventions focused on exercise training [19,23]. Furthermore, research studies about physical activity have a well-established bias of recruiting participants who are already active [24]. This study targets those who are not active but want to become active hence addressing the former limitation noted in previous studies.
Our team previously found that children with medical conditions and disabilities were motivated to take part in physical activity but lacked confidence in their ability to successfully participate (manuscript in preparation) confirming findings from existing literature [11–13]. These children and youth require support to develop a realistic plan that enables them to successfully move forward. As such, focusing on ways to set appropriate goals and develop a realistic action plan will build confidence around physical activity in this population to help them transition from the preparation stage of behaviour change to the action stage [14]. We have previously shown that physical activity plans with intensive kinesiology support can significantly enhance activity motivation, physical competence and daily physical activity participation among children with congenital heart defects, with the benefits maintained up to 5 years post-intervention [17,25]. Moreover, prior research has shown increased effectiveness of group-based physical activity interventions that use principles of group dynamics outlined by Carron and colleagues [26,27]. These group-based physical activity interventions have shown that, as the amount of contact and/or social support provided by researchers, healthcare professionals, and/or other exercise participants increases, so do the benefits of these activities when compared to individual physical activity interventions [28]. In adolescents with disabilities, exercising in group settings with youth of similar ages facilitated engagement in physical activity [29]. As such, we have designed a group-based intervention that utilizes this literature in a previously under-investigated population.
Study Objectives
The goal of the trial is to enable participating youth to move from the preparation to the action stage during the 12-week study intervention, leading them to adopt a more active lifestyle. The focus of this trial will be to equip youth with physical activity skills, goal setting and self-management experience, thus allowing them to more confidently participate in physical activities appropriate to their medical condition or disability.
Hypotheses
Our primary hypothesis is that children with medical conditions and disabilities, aged 8 to 18 years, randomized to receive 24 hours of healthy, active lifestyle support will have more confidence that they can participate in physical activity than those who do not receive support. Our secondary hypothesis is that, in comparison to the wait-list control group, those receiving kinesiology support will manifest a healthier lifestyle reflected in closer compliance to the Canadian 24-hour movement guidelines for a healthy lifestyle.
METHODS
This prospective, randomized 1:1, single blind, controlled trial (outlined in Figure 1) will enroll 128 children aged 8 to 18 years with medical conditions and disabilities. Randomization, stratified by sex and age groups (child 8-12 years / teen 13-18 years), will be assigned at study enrollment with outcome assessors blinded to group allocation. Ethics approval for this study was granted by the Research Ethics Board at the Children’s Hospital of Eastern Ontario (CHEO) (REB file #19/115X). Informed written consent will be obtained from the child and parent during their appointment in the outpatient clinic or over the phone for patients recruited using an out-of-clinic strategy. Children too young to provide consent will be asked to provide assent to the study activities. The study is registered at ClinicalTrials.gov (NCT04106154).
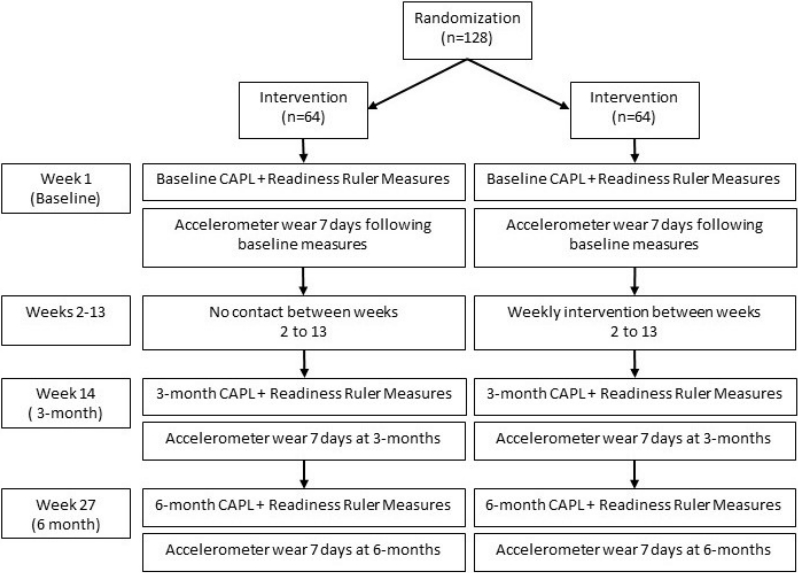
Physical activity support in youth with medical conditions and disabilities randomized controlled trial protocol outline
Abbreviation: CAPL = Canadian Assessment of Physical Literacy
Participant Recruitment
Participating clinics are the rehabilitation, chronic pain, endocrinology, respirology, spina bifida, cerebral palsy, post bone marrow transplant, genetic and metabolic bone disease and cardiology clinics at the Children's Hospital of Eastern Ontario (CHEO) and the ActiveCare Concussion Clinic (Ottawa, ON). Clinicians identified that these patient populations are likely to be motivated but not confident for physical activity. The research coordinator will work with pediatric subspecialists (co-investigators on this project) and allied health professionals in these clinics to initiate participant recruitment. Study eligibility and permission to approach the patient will be confirmed with the physician most responsible for the child’s care. Furthermore, given existing disparities around access to physical activity promotion and opportunities, various equity-deserving groups within the Ottawa community will be recruited and represented throughout the study.
Inclusion and Exclusion Criteria
Participants will be 8 to 18 years, who are actively followed in one or more of the participating clinics or those who are referred to the program by the healthcare professional responsible for their care. There must be physical activity concerns (i.e., concerns for lack and/or absence of physical activity) for the child, as identified by the patient, parent, and/or healthcare professional and the child must be able to participate in physical activity as specified by the responsible physician. Participants must score ≥ 4 points on the Motivation Ruler [30] for physical activity and ≤ 8 points on the Confidence Ruler [30] for their self-perceived ability to achieve a change in physical activity, or information provided by the parent indicates that the child lacks confidence for physical activity participation. Children who have an intellectual delay (such as, Down syndrome or low functioning autism) or an illness (such as, advanced Duchenne muscular dystrophy) that impacts their physical activity and/or that prevents them from completing the study assessments will be excluded. Presence of such conditions and whether a child can appropriately partake in the study will be assessed by the physician most responsible for the child’s care.
Sample Size
The study will recruit 128 participants, which will allow for 11% attrition; a rate similar to our previous kinesiology intervention studies, which apply knowledge of physical exercise and body movement to promote health and well-being [17,31]. We will examine the change in motivation and confidence total score over time (score, time, score*time) and adjust our model for five potential confounders: age group (child/adolescent), sex, study group (intervention/control), intervention format (in-person/virtual), and intervention compliance (% of intervention completed). Therefore, according to Green [32], a sample size of 114 patients (total sample = 50 + 8 patients x 8 variables/terms in the model) would enable us to evaluate our primary outcome and provide 80% power to assess for moderate differences in the physical activity motivation and confidence total scores between children in the intervention and control groups (alpha = 0.05). In discussions with the parents of potential study participants, we have found 50% would only participate if the intervention was delivered virtually. Another 40% of parents indicated that they would not want, or their child would not be successful in a virtual intervention, while 10% of parents would agree to either format. Pandemic restrictions have also greatly reduced the number of children who can attend each program. With a maximum group size of 10 people in the available indoor space, we can accommodate only 7 or 8 children in addition to the 2-3 staff required to lead and support participants. Although there are no limits to the number of children who can partake in the virtual sessions, to maintain standardization across groups, we plan to have the same number of children in each group intervention regardless of the delivery method (i.e., in-person versus virtual).
Study Assessments
The same assessor, blinded to study group randomization, will complete all assessments with all participants at three different timepoints: baseline, 3-months and 6-months. Of note, participants will be randomized to either an immediate or delayed intervention (i.e., control group). Children randomized to the control group will continue with standard clinical care (i.e., routine follow-up with the participants’ most responsible physician) and complete the three assessments at enrollment and 3 and 6 months before participating in the intervention, therefore minimizing the impact of randomization on study adherence and response.
Study Outcomes
The primary outcome will be the confidence subscore within the physical activity motivation and confidence domain total score from the Canadian Assessment of Physical Literacy [33,34] .This will be used to assess whether kinesiology support can increase the confidence of children with medical conditions and disabilities when it comes to physical activity and achieving a healthier lifestyle. The 12-item questionnaire contains four subscales which evaluate physical activity motivation and confidence: (1) self-perceived adequacy, (2) competence for physical activity, (3) predilection, (4) internal motivation for physical activity participation [35]. The former two subscales measure activity confidence and the latter two measure activity motivation. The motivation and confidence subscales of this tool have been shown to have good score reliability and validity evidence based on evidence of a factor structure [35]. For measures of adequacy and predilection, children will choose the sentences that are most like themselves. For competence and internal motivation, the child will be asked to rate themselves using a 5-point Likert-type scale (“Not like me at all” to “Really like me”)[34]. The total score from the two confidence measures will be the primary outcome.
Secondary outcomes
Motivation and confidence for changing health behaviours in general (not specific to physical activity behaviour), will be assessed using the previously validated Readiness Ruler [30], a previously validated tool [36]. The Readiness Ruler (also used to screen participants for the study) requires participants to rate their current motivation and confidence for behaviour change on a scale from 1 to 10.
Daily physical activity participation will be assessed by having children wear an Actical z-series omni-directional accelerometer (Phillips, Bend, Oregon, USA) 24 hours per day for 7 days [37]. Children who walk will wear the Actical over the right iliac crest [37]. Children who use a manual wheelchair for mobility will wear the Actical on their right wrist [38]. Actical activity measurements will be classified as sedentary, light, moderate or vigorous using established cut points [39]. For the same seven days, children will also complete a sleep and screen time log, indicating the time they awoke each day, the time they went to sleep each night, and their use of screens during their leisure time (i.e., excluding screen use during school classes or for homework). The accelerometer data classified as sedentary during the indicated timeframe when the child was in bed will be recorded as sleep time. The accelerometer results will be compared with the Canadian 24-Hour Movement Guidelines for Children and Youth [40] to evaluate guideline compliance.
Delivery of the intervention will be evaluated by tracking attendance and activity participation for each intervention session. The activities planned and completed during each session will also be recorded. Evaluating this information will provide important information on the ability to effectively deliver the in-person and virtual formats as well as the willingness and ability of children with medical conditions and disabilities to participate.
Kinesiology Intervention
This study will evaluate the impact of group sessions, comparing those delivered through in-person or virtual formats, for increasing physical activity confidence among children with medical conditions and disabilities. When comparing virtual versus in-person modes of delivery, it is important to note that they each have their unique advantages and challenges. Virtual physical activity interventions targeting children and youth can facilitate individualized and self-regulated learning, by personalizing the digital processes based on the individual goals and behaviour [41]. The format of the intervention will be selected by the patient/family. The option for virtual sessions was developed due to the varying COVID-19 pandemic restrictions and the limited willingness of some families to be randomized to an in-person intervention.
The kinesiology intervention is designed to increase patients’ physical activity confidence through a combination of physical activity participation and education sessions aimed at increasing physical activity knowledge, goal setting and self-management. The virtual intervention will provide the same exposure as well as the same balance of physical activity participation and educational activities. The intervention will be delivered in a group format and involve physical activities and education appropriate to each child’s medical condition and/or disability. The physical activity intervention is aligned with patient and family feedback (CHEO Family Advisory Council and Youth Forum) that emphasized that children wanted to attend sessions where they could not only learn about healthy lifestyles but also try various types of physical activity to see what activities they were able to do and wanted to pursue. This format has been previously used by our team to successfully introduce children and adults with congenital heart defects to various physical activities for each season of the year [31]. Based on the results of the former study, and the input received through consultations with the Family Advisory Council and Youth Forum, we designed the intervention for this study as a series of 12 weeks of group exercise sessions.
The in-person intervention will be twelve 2-hour weekly sessions, providing 80 minutes of physical activity participation and 40 minutes of educational activities, all of which will be led by the research coordinator (JY) to allow for a standardized intervention (Table 1). Undergraduate and graduate students learning physical activity counselling and behaviour change will assist the coordinator with session delivery. One two-hour session per week was designed to minimize family travel to the recreational facility. The virtual intervention will be 24 1-hour sessions held two days per week for 12 weeks. Each 1-hour virtual session will include 40 minutes of physical activity and 20 minutes of educational activities that the child can do at home while connected to the lesson. Two one-hour sessions per week was selected because of concerns that engagement in one two-hour virtual session would be limited. Both the in-person and virtual formats will provide a total of 24 hours of kinesiology support. Each week, participants will be guided to develop an individualized SMART (Specific, Measurable, Achievable, Relevant, Time-Bound) plan for changing their activity behaviour. Their weekly SMART plan will specify the home/ community activities they will do prior to the following week’s session. The study kinesiologist (JY) will also support each participant by conducting weekly calls to discuss progress towards activity goals. Through active participation, children will learn 2 to 4 physical activities per week that they can do with family or friends. Each session will consist of five components: an introductory activity, two physical activity sessions (e.g., music and creative movement), an education session (e.g., Canadian guidelines for healthy lifestyle), and a final session to establish the activity plan for the coming week. Intervention compliance will be evaluated by tracking session attendance and participant-reported completion of the weekly individual activity plans.
Randomization and Blinding
Randomization will be done with an equal allocation ratio of 1:1 (intervention:control) stratified by sex (female/male) and age group (child 8-12 years old/teen 13-18 years old) to allow for exploratory secondary analyses of whether the kinesiology support intervention is impacted by known differences in physical activity motivation by age and sex. The study biostatistician will generate the randomization. The research coordinator (JY) will have access to the randomization allocation after the participant has enrolled in the study. Study participants, their families, and the research staff running the intervention will be aware of the kinesiology support intervention as blinding is not feasible. Assessments will be completed by a researcher blinded to study group allocation. The data analyses will be completed by a statistician blind to group allocation.
Statistical Analyses
All statistical analyses will be performed using SPSS software version 28 (IBM Corp 2017). The between-study group baseline characteristics will be analysed using descriptive statistics: means, standard deviations, medians and inter-quartile ranges for continuous-type characteristics and frequency distributions for discrete-type characteristics. A two-sided alpha level of 0.05 will be used to determine statistical significance.
The Canadian Assessment of Physical Literacy (Version 2) confidence total score will be compared between the in-person intervention, virtual intervention and control groups over time using a repeated measures mixed model. The model will be adjusted for potential confounding variables (age group, sex, intervention compliance, and intervention format (in-person/virtual)) as fixed effects factors.
Difference scores will be calculated for the Readiness Ruler motivation and confidence measures, comparing baseline and 3-month assessments. ANOVA analyses will compare changes in scores between study groups (in-person, virtual, control). A secondary analysis using logistic regression will compare study group odds-ratios where the dependent variable is the Readiness Ruler confidence score (9 or more points vs less than 9 points) post-intervention (i.e., at the 3-month assessment timepoint) and the independent variables are the study group and the Readiness Ruler confidence score at baseline.
The impact of different methods of measuring daily physical activity will be assessed through a sensitivity analysis comparing waist- and wrist-worn accelerometers. If the pattern of daily physical activity changes across all study visits differs by measurement method, then only data for children with a waist-worn accelerometer will be included in the guideline comparison. The comparison of healthy lifestyle behaviours between study groups will be achieved by calculating the number of guidelines [40] achieved (Yes/No) during each assessment timepoint. The score will be calculated (0 to 4) based on achieving the guidelines for light activity, moderate activity, sleep, and screen use for each participant. Chi square statistics will be used to compare the proportion of participants achieving the guidelines for a healthy active day between the study groups for each timepoint (i.e., baseline, 3-months, and 6-months). Exploratory secondary analyses will examine whether the intervention effect is impacted by the known differences in physical activity motivation by age and sex.
DISCUSSION
This randomized controlled trial will evaluate the impact of kinesiology support in clinical care on the physical activity motivation, confidence, and participation of children between the ages of 8 to 18 years with medical conditions and disabilities in Ottawa, Ontario, Canada. The implications of this study are manifold. Firstly, this study offers a nonpharmacological and accessible way of encouraging healthy lifestyle behaviours and outcomes in children and youth with medical conditions and disabilities. Application of a personalized physical activity intervention appropriate to the participants’ medical condition and disability and the development of individualized SMART physical activity plans will enable patients to experience appropriate physical activities that minimize symptoms and optimize their physical and mental health benefits. Additionally, assessing compliance to the intervention depending on the delivery methods of the intervention (i.e., in-person vs virtual) may inform future research around implementation of physical activity interventions in a virtual setting, all the while maximizing long-term adherence in participants.
This study is not without limitations. Recruitment of individuals who are already active is a well-known bias in studies pertaining to physical activity as these individuals are more likely to volunteer. Given that this study targets individuals who lack the confidence to participate in physical activity, we will minimize this bias through our initial screening task. More specifically, eligible patients will be those who rate their confidence using the Readiness Ruler as being equal to or less than 8 out of 10 points. The results for individuals with a score higher than 8 may be influenced by a ceiling effect given that those scores indicate ongoing attempts at changing a behaviour whereas scores equal to or less than 8 represent readiness, uncertainty, and/or non-readiness to change [30]. To mitigate an increase in physical activity in response to study enrollment (Hawthorne effect), control group participants will be asked to maintain the same level of physical activity for the entire duration of the study. We will verify compliance with this request by examining the accelerometer data. We will enable participants to choose either the in-person or virtual intervention format based on their personal preference, and have accounted for an 11% attrition when calculating our target sample size. Furthermore, although the in-person and virtual intervention format are identical in content, a possible limitation of this study is the engagement of youth and therefore efficacy of the physical activity intervention for those enrolled in the virtual format. To mitigate the effects of the delivery format, final analyses will control for delivery format to assess for differences across subgroups. Finally, throughout the study, the accelerometer results will be compared with the Canadian 24-Hour Movement Guidelines for Children and Youth [40] to evaluate guideline compliance. A limitation, however, is that these guidelines were established based primarily on studies that did not include children and youth with medical conditions and disabilities.
CONCLUSIONS
This study will evaluate a physical activity intervention aimed at increasing the confidence of children living with a chronic medical condition or disability who are motivated to lead a more active lifestyle. The physical activity intervention was developed through clinical experience combined with patient/family feedback. The group-based intervention combines physical activity opportunities with education sessions that aim to enhance children’s understanding about appropriate physical activity and behaviour change. Through this study, children will gain experience engaging in and learning about physical activities they can successfully complete and that are suitable for their medical condition or disability.
Acknowledgements
We greatly appreciate the time commitment and collaboration from study participants, families and clinic and research staff. This research is funded by the Physicians’ Services Incorporated Foundation.
Notes
Conflicts of interest
The authors declare no conflicts of interest.

