Proceedings from the Ice Hockey Summit III: Action on Concussion
Article information
Abstract
Objectives
The Ice Hockey Summit III provided updated scientific evidence on concussions in hockey to inform these five objectives: (1) describe sport related concussion (SRC) epidemiology, (2) classify prevention strategies, (3) define objective, diagnostic tests, (4) identify treatment and (5) integrate science and clinical care into prioritized action plans and policy.
Methods
Our action plan evolved from 40 scientific presentations. The 155 attendees (physicians, athletic trainers, physical therapists, nurses, neuropsychologists, scientists, engineers, coaches and officials) voted to prioritize these action items in the final Summit session.
Results
(1) establish a national and international hockey data base for SRCs at all levels; (2) eliminate body checking in Bantam youth hockey games; (3) expand a behavior modification program (Fair Play) to all youth hockey levels; (4) enforce game ejection penalties for fighting in Junior A and professional hockey leagues; (5) establish objective tests to diagnose concussion at point of care (POC); and (6) mandate baseline testing to improve concussion diagnosis for all age groups.
Conclusions
Expedient implementation of the Summit III prioritized action items is necessary to reduce the risk, severity and consequences of concussion in the sport of ice hockey.
INTRODUCTION
Ice hockey is a collision sport played at high speed on a hard surface with rigid boards. The risk of concussion has been well documented [1-7] and potential sequelae, including chronic traumatic encephalopathy (CTE), are alarming. [8-13] The Ice Hockey Summit III: Action on Concussion brought together physicians, researchers, athletic trainers, sports scientists and engineers to describe sport related concussion (SRC) epidemiology, classify prevention strategies, define objective, diagnostic tests, identify treatment and integrate science and clinical care into prioritized action plans and policy. Presentations and discussion panels were organized to address the objectives before attendees selected the most highly prioritized action items. The purpose of this narrative is to share the information and propose strategies to reduce the risk, severity and consequences of concussion in the sport of ice hockey, similar to the Ice Hockey Summits I and II [1-4,14,15].
Objective 1. To Address Epidemiology and Psychosocial Influences on Concussion
Concussion susceptibility is influenced by intrinsic and extrinsic risk factor interactions. Modifiable intrinsic behaviors include balance/proprioception, physical conditioning, psychosocial and physical health status, whereas changeable extrinsic factors include rules, equipment, training volume and coaching. Risk factors should be considered before prevention programs are designed. Hockey, popular worldwide, currently has the following player participation and national percentages: Canada: 631,295 (1.8% of population); USA: 555,935 (0.17%); Czech Republic: 113,425 (1%); Russia: 105,059 (0.07%); Finland: 76,387 (1.4%); Sweden: 63,901 (0.6%); and Switzerland: 26,840 (0.3%). Concussion rates vary by level of participation (LOP) and diagnostic criteria used with incidences of 1.47-1.58/1000 athlete exposure (AE) for youth, 0.54/1000 AE for high school, 0.5-15.8 concussions/1000 AE)] for Junior A and in NHL, concussions range from 20 to 26% of all injuries [1.45-1.8 concussions (1000 AE)]. Helmets reduce head fractures and intracranial bleeds, but their function is influenced by design, material, fit, age, face shields, chin straps, and “J” clips. Mouthguards provide protection against dental injuries, but their role in reducing SRC is not scientifically demonstrated. Concussion severity based on time loss from participation is reduced modestly when full facial protection is worn and players compete on larger ice surfaces. Rule changes favor no-checking leagues and fewer non-injurious head contacts occur with ‘intensified’ compared to ‘non-intensified’ Fair Play rules [16]. No significant risk reduction resulted from the NHL’s zero tolerance for head contact rule. Rigorous hockey studies for concussion prevention testing of modifiable intrinsic and extrinsic risk factors, effect modifiers, exposure time (IET) and mechanism of injury are needed [3,17-20].
Psychosocial, psychologic, and psychiatric factors such as perceived vulnerability, willingness to report, incidence, symptom reports, time loss, playing style, and mental health issues influence SRC rates. Risks associated with gender, sport performance behavior, and mental health have been examined. Injurious hockey behavior increases during games compared to practices and psychiatric factors influence SRC outcomes. Players with a mental health history and recurrent SRC are at greater risk of depression. SRC clinical risk profiles include anxiety and mood disturbance characterized by hypervigilance, anxiety, and apathy. Psychosocial factors receive little attention in clinical practice literature despite their influence on SRC incidence and recovery. This omission demands further attention [21-25].
Objective 2. Head Impacts Causing Concussion: A Foundation for Prevention
A. Head Impact Biomechanics Informed by Helmet Sensors
The assessment of neurofunctional status after suspected concussion is typically based on subjective symptoms. Player assessments are influenced by awareness and honest reporting. Subjectivity impedes identification of biomechanical thresholds associated with SRC in players consenting to wear accelerometers. Sensors in helmets, patches and mouthguards report limited information on rads/sec2 head movement in SRC.
Head impact sensors monitor Head Impact Exposure (HIE) during practices and games [26,27]. These devices record impact frequency, magnitude, and location/direction that enable injury protection strategies and inform helmet design by level of play and gender [27]. Players experience HIE at all levels of play, including leagues that don’t allow body checking. HIE is sensitive but not specific to SRC diagnosis, confounded by subjective concussion diagnostics [19-22,26,27]. HIE enables identification of individual and team at-risk techniques from single and cumulative impacts that trigger medical evaluation, coaching, education, and rules changes. HIE technology assessment and brain injury risk (SRC) have been studied in American football (FB) [23,26,27] but data for hockey is sparse. Injury comparisons between FB and hockey can identify differences in SRC risk and injury mechanism. HIE hockey data has been obtained from Bantam and college players. Comparing Bantam players to same age FB players is more accurate than Bantam to college player comparison. FB players (11-14 years) have reported 252 impacts per player per season (PPS) [28], whereas Bantam and Midget hockey players (13-16 years) had an impact frequency of 223 per PPS [29]. Impact severity was greater in youth FB than hockey for mean linear acceleration (25.5g vs. 18.4g) and mean rotational accelerations (1691.8 rad∙s-2 vs. 1464.5 rad∙s-2). The 95th percentile linear head accelerations experienced by youth FB players (57.3g) was higher than hockey players (45.6g), but the rotational accelerations were higher in hockey. Game head impact frequency in same-age FB players occurred at 12.0 impacts per player per game (PPPG) versus 5.2 impacts PPPG among Bantams (13-14 yrs.) [30,31] Data suggest 13-14 year old FB players sustain greater HIE than age matched hockey players, differences that may influence SRC risk. A season of youth FB (13-14 years) was not associated with impaired clinical neurologic function [30,32] This finding might be similar in youth hockey players since they have a lower HIE. There is concern for the young athletes who participate in FB and hockey concurrently, which doubles their SRC risk exposure. Frequent repetitive head impacts separated by short recovery times predispose the brain to injury. Cumulative HIE must always be considered [23,33].
The relationship of head impact events to head accelerations in hockey is known. Falls, collisions, punches and projectiles cause linear, rotational, and/or angular accelerations that result in quantifiable tissue stress, strain, and strain rates. Magnitude and impact frequency are associated with SRC risk. Increased impact frequency is hypothesized to increase risk of developing CTE. In women’s elite hockey, falls cause 63% of head impacts and collisions 37%. In men’s elite hockey, collisions account for 80% of head impacts, fights 8%, and falls 7%. Video reconstruction of injury events and impact characteristics provide input into finite element modeling [34]. Linear accelerations to the head from falls are high, but a punch (uppercut) generates the highest rotational accelerations (rad/sec2) and likely results in diffuse axonal injury (DAI). Impact types dictate how energy is transferred to brain tissue [29]. The high linear (g) and rotational (rad/sec2) accelerations listed in Table 1 must be avoided [28,29,35-38].

Mean Peak Linear (g) and Rotational (rad/s2) Accelerations and Maximum Principal Strain with SD in Brackets for Each Mechanism of Injury
In summary, reducing HIE at all levels seems practical. Inadvertent head impacts in ice hockey will occur, but purposeful use of the head or involvement of the head during or subsequent to play should be aggressively removed from the sport. HIE can alert coaches and sports medicine providers when worrisome on-ice or locker room events occur.
Video Reconstruction Determines Concussion Causation
Biomechanical analysis of SRC impacts connect head trauma to mechanical responses of brain tissue. SRC detection requires valid measures to assess brain tissue trauma, including impact characteristics: (i) velocity, (ii), compliance, (iii) location, and (iv) impactor mass. Video reconstruction (VR) accurately obtains impact parameters, including direction. VR depicts relationships between (a) linear and rotational accelerations and tissue trauma; (b) the effect of and duration of impact events on tissue trauma, and (c) the relation between brain tissue trauma and SRC risk. Impact frequency and linear acceleration contribute less to understanding SRC in hockey, but provide valuable measures of brain tissue strain, quantification of tissue involved, location and time intervals between events and head trauma duration. These parameters are critical to evaluating sustained trauma and managing subsequent SRC signs and symptoms. Relating dangerous impacts to brain tissue damage such as SRC are valid contributions video reconstruction provides to our understanding of hockey SRC. This information contributes to the development of SRC prevention strategies [19,28,36,39,40].
B. Preventing Concussion
Concussion prevention tactics include: neck strengthening and anticipation, removal of body checking, behavioral modification (i.e. Fair Play), elimination of fighting and financial incentives in the NHL to discourage dangerous activities.
(i) Neck Strength and Anticipation: Neck strength and concussion awareness may reduce SRC risk and severity [41]. Strong neck muscles [42] contracted in collision anticipation can decrease kinematic head response to external forces. A benefit occurs when extension of effective moveable mass (the head) moves from neck to torso. Improved neck strength occurs from diverse strengthening programs after short time periods. Reduction of SRC risk and severity from stronger neck muscles remains to be proven. Collins followed 6,704 males and females in soccer, basketball and lacrosse. Increased neck strength (measured by hand held dynamometer), decreased concussion odds by 5 percent [16]. Conversely, when Bantams wore HITS helmets, increased cervical neck strength (CNS) did not reduce linear (g) or rotational (rad/sec2) accelerations [43]. Differences may be explained by subjects, reporting, and measurement methods. Dynamic stiffness, the ability to resist movement from a perturbation force, and hit anticipation were more influential than muscle strength alone [16]. Increased stiffness and cervical muscle contraction, when anticipating a “hit” reduces subsequent head movement. Contraction of the cervical muscles that affix the head to the trunk decreases post-impact head movement/acceleration and reduces SRC risk and severity. Future studies must investigate programs to improve neck strength, muscle performance, and cervical spine dynamic stiffness, in addition to testing the premise “head on a swivel.” These data support penalizing infractions such as checking from behind (CFB), open ice unanticipated and blind-side hits that impede players from pre-emptive neck muscle contraction [6,16,42-47].
(ii) Body Checking: SRC is reduced by eliminating body checking (BC) in Pee-Wee and ensuring abstinence or optimal checking in Bantams. A three-time greater risk of injury and a four-time greater risk of SRC in Pee-Wee BC leagues compared to non-BC leagues have been reported. BC is a consistent risk factor in youth hockey concussion due to discrepancies in player maturation (height, weight and skill development). Implementing no BC in Pee-Wee reduced SRC by 67%, a positive finding that must be extended to Bantams.
(iii) Fair Play: In 1979, Vaz introduced Fair Play (FP) in Quebec to improve hockey safety using behavioral modification (rewards and punishment) to counter both violence and declining participation [48]. Teams earn two points for a win, one for a tie, zero for a loss, and a single FPP is awarded for respectful play: available to both winning and losing teams. Excessive penalty minutes by a team (age adjusted), unsportsmanlike behavior by a player, parent or coach can result in forfeiture of a team’s FPP. Studies looking at injury rates, including concussion, show a decrease in these injuries in tournaments played under FP rules [49]. In assessing injury rates there is evidence suggesting that teams forfeiting their FP point (suggesting a less disciplined style of play) experience a higher injury rate compared to teams that earn their FP point [8,50-53].
(iv) Fighting: Although not a major cause of SRC in youth or high school hockey, the complete elimination of fighting in the sport is mandatory. Many players in youth, high school and Junior A aspire to play hockey at higher levels, which motivates them to engage in fighting by taking lessons, practicing in locker rooms, hotels, and sometimes on-ice. No fighting should occur at any level because of the immediate and potential long-term consequences, such as CTE [8-10,44,54]. A punch to the face has been shown to cause some of the highest recorded rotational accelerations and is clearly a very high-risk mechanism for concussion.
(v) Can Financial Concerns and Litigation Reduce Concussion?: A retrospective cross-sectional study of 323 non-career ending concussions in NHL players (2009 to 2012) showed NHL salary losses of $42.8 million occurred annually. Payment to retired players over a 20-year period cost the NHL $135 million. Assumptions that aggressive hockey, including fighting, generates NHL revenue by increasing game attendance, may explain why recommendations to reduce head trauma in professional hockey have been ignored. Such arguments might be countered by (i) salary expenses from absent and retired SRC players, (ii) medical costs to treat head injuries, (iii) lost ticket sales and television revenue when star players are sidelined, (iv) criticism of the NHL when their SRC stance is publicized, and (v) the financial toll of SRC on the NHL is significant [9,46].
Objective 3. Diagnosing Concussion: What Tests are Reliable and Evolving?
It is imperative that the pathophysiology of concussion is understood prior to diagnosing. SRC pathophysiology relates to clinical findings, injury response, and recovery time. SRC is manifested by (a) ionic flux and neurotransmitter release; (b) neurometabolic cascade and energy crisis; (c) axonal dysfunction and injury; (d) synaptic dysfunction; (e) blood brain barrier and cerebral blood flow changes; (f) glial reactivity and neuroinflammation; (g) impaired glymphatic clearance; (h) altered protein homeostasis and (i) potential neurodegeneration [10,54]. Post-SRC dysfunction may manifest as migraine symptoms, impaired cognition and processing, lack of coordination, behavioral changes, CBF changes, slowed learning and plasticity. Imaging post-acute mTBI shows (CBF) alterations may outlast symptoms and neurocognitive impairment (NCI). SRC neurobiological response progresses from seconds to minutes with full recovery requiring weeks or perhaps longer. Studies are clarifying links between acute SRC pathophysiology progression to chronicity and neurodegeneration (CTE, Parkinson’s Disease and Alzheimer’s Disease). The Mayo Clinic Ice Hockey Research team developed an evolving Objective Diagnosis of Concussion. Although that data is collected at rink-side, it is not yet used in initial diagnoses. As such, clinical diagnoses at rink-side and medical diagnoses made in clinic are appropriately discussed first [10,54-57].
Diagnosing Concussion in Players at Rink-Side
Ideally, a hockey knowledgeable, trained medical professional (athletic trainer, physician, physical therapist) is present to assess players suspected of SRC and reduce risks of returning concussed players to play. Experienced providers astutely observe mechanism of head impacts and subsequent player behavior. Baseline testing pre-season provides comparisons for subsequent assessments, including a symptom scale, cognitive and balance tests (Sideline Assessment of Concussion Test- SCAT5) and rapid number naming tests (King-Devick Test). Players are removed from the game or practice if findings are consistent with SRC: observed mechanism of injury, signs, symptoms, abnormal physical exam, cognitive, balance or oculomotor tests as compared to baseline [54,55,57-59].
Diagnosing Concussions and Determining Severity in a Medical Setting
Despite promising biomarkers, an SRC clinical diagnosis requires a focused and relevant history and examination. Important is timing, mechanism, head impact location of current SRC, symptoms and signs including loss of consciousness, amnesia, risk factors, post-SRC sequelae, and a history of previous concussions and the duration of symptoms. If a prior history of concussion exists, lower SRC acceleration thresholds (lesser magnitude of impact) will result in concussion. Only 50% have symptom severity scores (SSS) of zero at baseline, supporting mandatory baseline assessment. Firm recommendations on which specific baseline tests will require validation for different groups, proper testing conditions, use of appropriate normative data and consideration of practice effects are needed. Currently, documented meaningful change is 6 points on the SSS. SCAT-5 contains a useful cognition test [sensitivity 64-89% and specificity 76-91%]. The Montreal Cognitive Assessment (MoCA) and computerized NP assessments (i.e. Cogstate or ImPACT) can supplement the SAC. Portions of the neurologic exam are core to SRC office evaluations. Assessing dynamic balance and vestibular function (e.g. timed tandem gait), oculomotor function (King-Devick Test, convergence insufficiency), and vestibulo-ocular reflex (dynamic visual acuity, head impulse test) are essential elements in the office examination of a SRC. FDA approved devices to assess balance now include Sway balance and a King-Devick balance test app [60-67].
Motor Impairments and Musculoskeletal Injury Risk after Return to Play
Accumulating evidence suggests post SRC athletes have sub-clinical deficits in neurocognition and neuromuscular control after a concussion, resulting in an increased risk of subsequent lower extremity injury (LEI) after return to play (RTP). Additional studies of cognitive and motor performance during dual-task conditions showed that concussed athletes demonstrate ongoing impairments in gait and balance even when performance on standard clinical measures had recovered [68]. RTP assessment of concussed athletes must include clinical tests of neuromuscular responsiveness under challenging sport-like conditions [61,68,69].
Importance of Objective Diagnoses of Concussion
Objective components of an SRC diagnosis (King Devick Test, QEEG and promising fluid neurobiomarkers shown in Figure 1) are aligning in research with SRC signs and symptoms. These tests need further validation before they can be relied on for diagnosis or to guide management of hockey SRC. The Berlin Consensus (or work by McCrae) identified similar components of promising measures emerging for clinical diagnoses and to guide and ultimately evaluate treatment effect [60,67,70-72]. Valid, objective diagnositic tests are needed to reduce either unreported (denied) or the opposite (exaggerated) symptoms and signs of SRC. Adding criteria to help determine diagnostic clinical certainty of concussion – definite, probable, possible – has been proposed.
Using the King-Devick Test in Concussion Diagnosis
Eye movement and vision related tasks involve 55% of brain pathways integral to brain integrity and are vulnerable in SRC. Rink-side SRC evaluation includes oculomotor assessment that contributes valid, critical, and objective data with greater accuracy and speed than balance and cognitive tests alone. Many SRC are not witnessed and over 50% of athletes don’t report SRC symptoms. The King-Devick Test (KDT) is a fast, valid, reliable, rapid number naming test that objectively identifies post-SRC suboptimal brain function. A meta-analysis of KDT data showed 86% sensitivity and 90% specificity for SRC, with five times greater risk of SRC (RR=4.92) if KDT time and accuracy worsens between baseline and SRC testing. KDT successfully distinguished between concussed vs. control in youth and collegiate athletes (ROC: KDT 0.92; TTG 0.87; SAC 0.68). A three-year study of rugby players demonstrated six times more unwitnessed/unreported concussions than witnessed SRC. All were identified with KDT (100% sensitivity, 94% specificity) including players with no clinical signs or symptoms. KDT is reliably administered by medical professionals as well as trained non-medical individuals, such as coaches and parents [67,73-76].
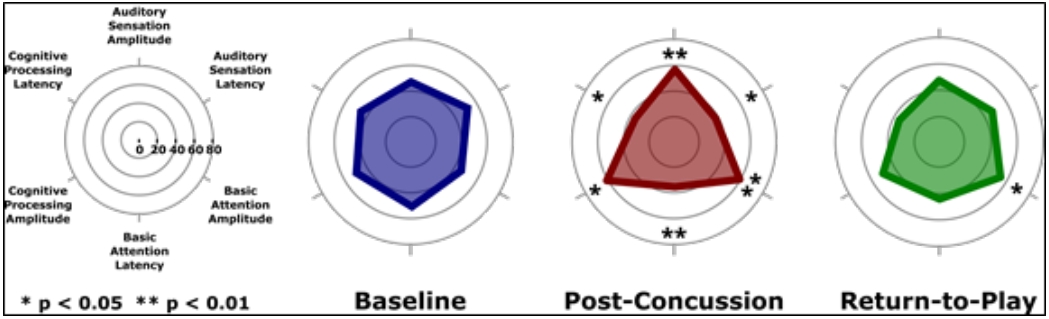
Quantified EEG (QEEG)
The objective evaluation of brain vital signs is possible with portable electroencephalography (EEG). Derived from established event-related potentials (ERPs) (i.e. N100, P300, and N400) provide a fast and automated evaluation of brain wave responses normatively quantified. Brain function changes in 47 Junior A hockey players post SRC were evaluated using a repeated measure design (baseline, post SRC, return-to-play (RTP), and post-season). SRC was hypothesized to cause significant changes in response amplitude and latency proving that brain vital signs are significantly changed after a SRC. Differences between baseline and RTP indicated persistent impairment despite a lack of clinical detection. Interestingly, significant sub-concussive changes in brain vital signs for pre- and post-season testing of players who did not sustain SRC further suggest enhanced sensitivity to concussion-related effects on brain function. Radar plots (Figure 2) showed systematic changes across six brain vital signs scores depicted by a unique ‘profile’ when baseline hexagonal shape transforms into a triangular shape, due to consistent increases in amplitude and decreases in latency for SRC. Support is evolving for the use brain vital signs as an objective, physiological measurement of SRC [24,77,78].
Fluid Biomarkers
Identifying objective biomarkers from neuronal, axonal and astroglial injury may aid SRC diagnosis [70], assess severity and predict prognosis. In addition, biomarkers in blood [66] or saliva may help determine potential long-term consequences of repetitive sub-concussive blows, recurrent SRC, and progressive neurodegenerative disease. Objective neurobiomarker results post-SRC will support medical personnel counseling at-risk SRC individuals. McCrea and colleagues reviewed the role of biomarkers in assessing SRC [60]. Eleven of 16 studies (14 blood + 2 saliva) showed that biomarkers aid SRC diagnosis (AMPAR, S100B, T-Tau, marinoburagenin, PSCPP, GFAP, NSE, SNTF, tau-C, metabolomics profiling). Although four showed evidence in predicting outcomes (SNTF, quinolinic acid, prolactin, tau-A), the level of evidence for fluid biomarker utility in clinical assessment of SRC was rated as low. MicroRNA, comprised of short, noncoding nucleic acids that regulate protein expression, travel through extracellular fluid in exosomes and are detectable in saliva. MicroRNA is functionally related to genes in the brain and values are altered after SRC, reflecting symptom character and duration. Blood and salivary biomarkers may play a role in SRC diagnosis, severity, prognosis and RTP decision-making. They are important research tools requiring further validation before they can be relied on for a SRC diagnosis or severity prediction [60,66,70].
Metabolomic Profiling
Significant acute symptoms may linger after a SRC, manifested by chronic long-term neurologic dysfunction (Post-Concussion Syndrome- PCS). Concussion diagnosis and return to play decision-making are difficult. Plasma metabolomic profiling as a diagnostic tool indicates SRC in youth hockey players can be accurately diagnosed (>90% diagnostic accuracy; P<0.0001). SRC causes a specific metabolomic pattern characterized by decreased plasma glycerophosopolipids. Metabolomics data were supported by MRI showing diffusion abnormalities within multiple white matter tracts, functional hyper connectivity, and decreases in choline 3 months after concussion. Metabolomic profiling, together with multivariate statistical analysis and machine learning, represents a novel diagnostic method for SRC that may be amenable to future point-of-care testing. These diagnostic tests are not yet ready for clinical application, but show promise for prompt SRC identification and severity prediction [11,79].
Contributing Consultations - Use of Neuroimaging
Computed tomography (CT) is the preferred imaging modality for moderate and severe neurotrauma to detect hemorrhagic intracranial lesions including intraparenchymal hematomas, subdural and epidural hematomas, subarachnoid hemorrhage, in addition to facial and skull fractures. However, diffuse axonal injury and petechial hemorrhages resulting from a concussion are not apparent on CT. Advanced MRI techniques characterize traumatic brain injuries in these CT negative lesions. Studies show reduced brain volume, even in subjects with normal T2 imaging. Focal reduced volume of the left cingulate negatively correlates with post SRC anxiety and other symptoms. Diffusion imaging (DI) has been shown to demonstrate lower fractional anisotropy (FA) with more significant changes in the temporal and occipital lobes. These FA changes are associated with significantly poor memory scores. Diffusion tractography demonstrates reduced tract size and focal disruption in fiber bundles. Functional MR demonstrates network activity disruption following mTBI. Also, increased functional activity has been shown post SRC. This increased activity reflects that higher levels of brain activity are required to perform memory tasks competently as well as normal controls. MR spectroscopy provides a quantitative measure of brain injury and can identify functional abnormalities in normal-appearing athletes post mTBI. N-acetylaspartate (NAA), a measure of neuronal health, decreases in SRC. NAA to creatine ratios have been proposed as a method to acutely assess severity of brain injury and follow recovery. Brain biomarkers detectable with advanced MRI techniques are helpful to understand the impact of SRC. Future research must focus on metrics to evaluate individual athletes post SRC in acute care settings. Accurate imaging techniques to detect mTBI and subsequently to confirm recovery are important steps forward in the care of SRC [80-83].
Session #5 – Expert Panel Ideas for Action on Concussion Panels
Nine experts, including health care professionals, former NHL hockey players, and USA Hockey’s coaching, officiating and safety leaders shared their hockey concussion experiences. These panelists bridged the gap between sophisticated medical knowledge and the harsh realities of competitive hockey. For example, an NHL player was asked if he openly admitted to his concussion symptoms and he replied “What, are you kidding, and lose my job?”
Objective 4. Taking Science and Treatment Forward: From Bench to Clinic and Rink-side
In Vitro Models for Brain Injury
In-vitro experimental models capable of finely controlling forces and deformations exerted on cells must be developed in order to understand mechanical force effect on neuronal health and function when head injury (SRC) occurs. Methods proposed include: physical impact, fluid percussion, fluid shear stress, and high-speed stretching models. These models consistently show mechanical injury leads to focal swelling, indicative of diffuse axonal injury. However, connections between head injury trauma and lasting dysfunctional chronic traumatic encephalopathy (CTE) are not known. Neurofibrillary tangles accumulating where large stresses are expected post head injury, suggest a direct connection between cell trauma and CTE development. In vitro models of mechanically induced dysfunction, combined with computational modeling of brain deformation during head injury could provide important insights into concussion pathways and potential treatment to prevent CTE in concussed hockey players [84-88].
Using Hockey Accelerations to Examine an Animal Behavioral Model
Injury risk curves relate neurofunctional status following exposure to biomechanical events (i.e. applied forces or head movement). Animal laboratory models can test SRC risk relationships to rapid head rotation, magnitude and direction and to influences of age, sex, and previous SRC on biomechanical SRC thresholds. TBI animal models exhibit LOC, axonal damage, hemorrhage and focal contusions in contrast to the subtle, subjective, cognitive, neurofunctional alterations found in players with SRC. Animal models provide insight into how head impacts and sudden head movements produce brain deformations that cause brain injuries (mTBI to TBI). Emerging research in objective, involuntary neurofunctional metrics and biomarkers are bridging gaps between human and animal research. SRC biomechanics provide a rational research foundation to test hockey SRC prevention strategies [89-93].
Pharmacologic Interventions Available Now and on the Horizon
Concussion is a complex multiphasic brain injury initially caused by a blunt force, followed by secondary injury involving meningeal and parenchymal inflammation, generation of reactive oxygen species, glutamate excitotoxicity, blood brain barrier (BBB) permeability, microglial activation, neutrophil infiltration, cellular edema, axonal injury, microtubule disassembly, and apoptosis. Biochemical and molecular factors involved in these injury cascades are targets for acute therapy to minimize/prevent secondary injury and mitigate neurological sequelae. Therapy to decrease inflammation and minimize secondary cascades aren’t available, thus research on treatment should be an SRC priority for investigators.
The secondary cascade (inflammatory oxidative crisis) causing cell death can be reduced by glutathione in concussion animal models. Pre-clinical evidence suggests the calcitonin gene-related peptide (CGRP) pathway may be a new target for drugs and monoclonal antibodies, especially for post-concussion headache. Preclinical and preliminary human evidence of efficacy for N-acetyl-cysteine (NAC) has been demonstrated to reduce post-concussion symptoms in a controlled study of military operators who sustained a blast-injury related concussion. In 2016 a study of thioredoxin-mimetic peptides, (TXM peptides) reported protection of cognitive function post mTBI in mice [94]. Astaxanthin also improved cognitive performance post mTBI in animals; this dietary carotenoid protects via anti-inflammatory and anti-oxidants (Ji X et al, Brain Research 2017) [94-99].
Fish Oils, Supplements and their Neuroprotective Effects
SRC induced by any forces to the brain may lead to symptoms and/or signs with or without loss of consciousness (LOC). SRC is predominantly functional despite the fact that neuropathological changes occur. SRC increases metabolic demand, impaired metabolism, decreases CBF and results in hypometabolism with symptoms persisting from 1-4 weeks. Nutritional supplements are hypothesized to provide neuroprotective/therapeutic effects. Ecosapentaneoic acid (EPA) and docosahexaenoic acid (DHEA) are omega-3 fatty acids found in human neuronal and synaptic vesicle plasma membranes involved in inter and intracellular signaling. These fatty acids influence apoptotic death via gene expression modulation. Several animal studies demonstrate post mTBI protective effects of DHEA & EPA alone or in combination. Animal model studies demonstrate recovery following TBI with DHEA and EPA supplementation. Other supplements with strong anti-inflammatory (curcumin) or antioxidant properties, such as resveratrol, melatonin and S. Baicalensis also show improved post-concussion recovery in animal models. Creatine, vitamin C, and vitamin E improve TBI outcomes in humans, but have not been evaluated in SRC. Vitamin D enhances TBI outcomes in animal and human studies when combined with progesterone, a combination not yet studied in SRC. Preliminary animal and severe TBI human studies are promising; however, current evidence does not prove that nutritional supplements prevent or effectively treat SRC [100-105].
Post-Concussion Syndrome (PCS)
The Fifth International Conference on Concussion in Sport (2016) defined PCS as an mTBI with symptoms persisting >14 days for adults and >4 weeks for children. PCS contributors include symptom severity, previous concussion, migraine, psychiatric history, adolescence, and female sex. Symptoms include headache, fatigue, noise or light sensitivity, dizziness, imbalance, disturbed sleep, irritability, emotional lability, anxiety, depression and inattention, concentration, memory, and thinking quickly. Structural brain and cervical injuries, chronic headaches, pain, vestibular and/or sleep disorders, depression, anxiety, adjustment disorders, ADHD, medication side effects, or drug and/or alcohol abuse must be excluded. PCS evaluation requires a comprehensive history of injury mechanism, initial and current symptoms, interval treatment, and medical and concussion history. The examination should address the vestibular, oculomotor, cervical spine and neurologic systems. Neuropsychological (NP) testing identifies cognitive, behavioral, and affective deficit severity to establish a baseline to track recovery. Aerobic exercise without symptom exacerbation is recommended. PCS patients may have reduced exercise capacity with shorter duration, higher perceived exertion and lower heart rate. Neuroimaging (fMRI, DTI, MRS), blood biomarkers, genetic testing, and QEEG are promising adjuncts to evaluation. Current PCS management requires medical, physical, and psychosocial assessment using a multidisciplinary, patient-centered approach. Educational materials (verbal and written), school accommodations, physical rehabilitation (symptom limited, personalized aerobic exercises, targeted vestibular, visual, proprioception and musculoskeletal (cervical spine) therapeutic exercise, and psychological consultation (reassurance, anxiety/stress management and cognitive, behavioral therapy need to be addressed. Cognitive rehabilitation emphasizes compensatory training, “brain breaks,” and coping strategies. Non-pharmacological methods initially treat headache, sleep, and mood disorders. Medications with sedating side effects must be avoided, whereas education and reassurance are central to concussion management and the player’s gradual return to activity [106].
Session #7 – Evolving Scientific Contributions
Effective Exercise Regimens for Post-Concussion Benefit
SRC adversely affects the autonomic nervous system (ANS) and cerebral blood flow (CBF) control. Guided aerobic exercise benefits blood pressure, CBF control and C02 sensitivity in post SRC-PPCS. Although evidence-based treatment is on the horizon for acute SRC, consensus-based recommendations emphasize rest until asymptomatic. New evidence suggests excess rest prolongs recovery whereas moderate physical activity (PA) one-week post SRC may reduce post-SRC- PPCS incidence. A systematic evaluation of exercise tolerance (Buffalo Concussion Treadmill Test) in players with PPCS followed by prescription of a controlled, sub-threshold exercise regimen showed a safe, speedy recovery. Preliminary data show sub-threshold exercise may speed recovery if administered the first week post SRC. This finding challenges the recent world consensus recommendation that athletes rest post SRC until symptoms stabilize. Athletes should be active but remain below cognitive and physical symptom-exacerbation thresholds. Strict abstinence of activity beyond a few days post-concussion is likely detrimental to SRC recovery. Moderate activity and aerobic exercise below symptom exacerbation appear safe, may speed recovery, and potentially prevent post SRC players from developing PPCS. Medication, supplements and exercise are promising, but preventing initial and recurrent SRC is most important [107-111].
Concussion Awareness: Positive or Negative for Concussion?
Concussion awareness has increased in sports including hockey, yet its effect across hockey participation age groups is not known. Although youth sport registration has increased across decades, some sports have recently experienced attrition. (#61–DS) Participation variation may be attributed to economic issues, increased specialization, and SRC. Participation in youth and high school FB along with sports with similar SRC risk have decreased. The national increase in hockey participation (#62, #63 – DS) may be attributed to better education for hockey stakeholders, including athletes, parents, coaches and medical providers. Despite a decade of youth hockey growth, 2011-2013 registration rates dropped locally and nationally. A potential explanation may have been the NHL lock-out and concurrent reports of concussion and neurologic injuries. Hockey participation rates continue to increase and may be influenced by concussion education, rule changes, and behavioral modification [112-115].
Opportunities and Barriers to Eliminate Fighting from Hockey
Fighting in hockey is learned and sustained by role modeling. NHL and Junior A hockey leagues tolerate fighting despite the fact that fans studied across 13 years favored skilled play and ‘no fighting’. The act of fighting causes repetitive head impacts and traumatic brain accelerations that contribute to SRC. Concern about the frequency and consequences of SRC provide opportunities to eliminate fighting and reduce head hits at all levels of play. Currently, proud Junior A players track their fights on www.hockeyfights.com. Repeated head trauma effects, including suicides in players whose role is to fight should be viewed through the lens of the neurometabolic cascade. Head hits in hockey create an oxidative crisis, diffuse axonal injury and may contribute to the develpmnent of CTE. All head trauma is harmful, but a punch delivered at an angle and a fall to the ice without a helmet result in some of the highest rotational accelerations. Zero tolerance for all head trauma requires rigorous rule enforcement and a fundamental change in hockey. Reducing head trauma requires the elimination of fighting, checking from behind, boarding, elbowing and locker room boxing (LRB). A designated individual on each team (Coach or “Safety Parent”) should supervise player locker rooms at every home and away games. Annual pre-season Safety Clinics can reinforce these messages. Fair Play expansion, elimination of body checking at the Bantam level and automatic game ejection for fighting were prioritized at the Ice Hockey Summit III (2017). Neurolaw will help apply scientific advancement to improved concussion policy [40,70,84,116,117].
The International Ice Hockey Federation (IIHF), International Olympic Committee (IOC), Federation Internationale de Football Association (FIFA), World Rugby Association and Federation Equestre Internationale (FEI) hosted 30 concussion experts and 410 participants in 2016 for a two-day conference. The experts developed guidelines from a systematic literature review, meeting discussions and consensus building. Emphasis was placed on concussion education, detection and prevention [118].
The Role of Science in Society: Research, Education and Practice
State concussion laws help translate emerging scientific knowledge into SRC policy. Following Washington’s lead in 2009, fifty states have enacted a youth SRC law. Each research community must partner with stakeholders, to ensure accountability. A policy challenge is facilitating accurate communication of risks and benefits to inform athlete and parent decisions. Accomplishing that objective mandates stakeholders to understand SRC statutes and think creatively about next steps. All stakeholders must work as a team and strive to improve youth SRC policy, guided by five foundational principles: Collaborative, Feasible, Scientifically Sound, Fidelity of Implementation, and Alignment of Incentives. Evaluation requires the alignment of incentives of schools and youth leagues to maintain high levels of participation. Challenges pertain to “fidelity of implementation”, which assesses how stated policy is executed in practice. What is written is often not followed. For instance, in on-going NHL litigation, medical staff clearly diverge from SRC protocols in some pressured situations. Variation is expected in youth hockey, and research is designed accordingly. There is also a potential for regional, socioeconomic, and racial variation in implementation of SRC hockey policy. [119]
Three panels interspersed during the Summit contributed significantly to the curriculum: Panel A comprised of three former NHL hockey players with previous history of significant concussion who discussed solutions. Panel B engaged three medical providers with hockey concussion expertise to obtain their ideas to address the concussion epidemic. Panel C benefited from the experience of USA Hockey Directors of Officiating, Coaching Education and Player Safety.
Objective 5. Integrating Science and Clinical Care into Our Action Plan
Acknowledgements
Drs. Stuart and Smith express their appreciation to Pam Otterbein, Sierra Tollefson, and Linda Gochnauer for their preparation for and execution of the Summit III. Thank you to Kevin Koenings who obtained seamless audiovisual prsentations for speakers presenting in person and for those presenting from elsewhere. Drs. Chip Burke, Michael Joyner, William Roberts, Chad Eickhoff, ATC, MsC, and Shaun Fickling are thanked for their medical and scientific advice. Drs. Nicole LaVoi and James Whitehead capably presented on social media and initiating take away messaging. Shjon Podein gave a thoughtful and memorable personal account of his professional hockey career. We appreciated panelists Mike Eaves, Michael B. Stuart, MD, Jordan Leopold, Matt Leaf, Mark Trabrum and Kevin Margarucci. Thank you to our supporting organizations: USA Hockey, International Ice Hockey Federation (IIHF), Thorne Science, Hockey Equipment Certification Committee (HECC), American College of Sports Medicine (ACSM), Johannson-Gund Endowment, Brian Mark Foundation and our Martineau Gift.
Notes
Conflict of Interest
The authors declare no conflict of interest.