Effect of Upper Limb Proprioceptive Neuromuscular Facilitation with Resistance Training on Respiratory Muscle Strength in Quadriplegics: A Randomized Controlled Trial
Article information
Abstract
OBJECTIVES
Spinal cord injuries lead to impairment of the respiratory system due to paresis or paralysis of the respiratory muscles leading to respiratory insufficiency, which is dependent on the level and completeness of the injury. The aim of this study was to evaluate the effect of upper limb proprioceptive neuromuscular facilitation (PNF) combined with resistance training on respiratory muscle strength and perceived difficulty of breathing in individuals with tetraplegia.
METHODS
26 participants with traumatic tetraplegia C5-C8 participated in the study. They were then allocated in two different groups. PNF Group received upper extremity PNF combined with resistance training for 10 repetitions per set, 3 sets 3 times a week for 4 weeks, and CONT Group received respiratory training with triflow type incentive spirometer. Participants were evaluated for maximum inspiratory pressure (MIP), maximum expiratory pressure (MEP) and modified borg scale (MBS).
RESULTS
After four weeks of intervention, there were significant improvement in the scores of MIP, MEP, MBS in both groups separately. Also between group comparison showed significant improvement in scores of MIP (P=0.004), MEP (P=0.004), MBS (P=0.001) in PNF Group as compared to CONT Group.
CONCLUSIONS
This study concludes that there was significant improvement in respiratory muscle strength and rate of perceived difficulty of breathing using upper limb PNF combined with resistance training in tetraplegics.
INTRODUCTION
Respiratory complications are the most frequent cause of morbidity and mortality in patients with tetraplegia [1]. Weakness or paralysis of respiratory muscles leads to decreased inspiratory force, decreased vital capacity, sputum retention and reduced ability to cough [2]. Patients with tetraplegia have restrictive ventilatory impairment, leading to a reduction in chest compliance by shortening and stiffening of the upstretched tissue and fibrosis of the weakened muscles [3].
The respiratory muscle dysfunction in tetraplegia can be due to muscle weakness (low maximal strength) or muscle fatigue (endurance capacity), which may have an impact on the activities of daily living [4]. In addition, it is well established that persons with tetraplegia have reduced physical capacity and relatively inactive life style that impacts the quality of life in these patients [5]. Dyspnea is common during activities of daily living [6] and studies show that strengthening of respiratory muscles could improve these symptom [7].
Impaired respiratory muscle function and increased risk of respiratory complications are indicators of respiratory muscle training in individuals with spinal cord injury (SCI) [8]. Several methods such as inspiratory muscle trainer [9], incentive spirometer [10], electrical stimulation of abdominal muscles [11], positive expiratory pressure therapy, breathing exercises such as diaphragmatic breathing, weighted exercises [12] have been used to improve strength of respiratory muscles.
Proprioceptive neuromuscular facilitation (PNF) is one option widely used in neurorehabilitation for strengthening. Among the PNF principles, irradiation is helpful especially for patients with muscle weakness in area that cannot be directly strengthened [13]. Stimulation of strong and preserved muscles groups produce strong activation of injured and weak muscles, thus facilitating muscle contraction [13]. Studies found that there is significant increase in respiratory muscle strength after a month of training with PNF combined with elastic resistance bands in normal healthy individuals [14]. In SCI individuals, respiratory muscle weakness s the primary cause of increased work of breathing, shortness of breath, reduced chest expansion and increased energy expenditure. Training of inspiratory muscles of respiration is essential to reduce respiratory complications. Techniques such as PNF have been proven effective for strengthening muscles in the past. Hence, the purpose of this study is to evaluate the effect of upper limb PNF combined with resistance training on respiratory muscle strength and perceived difficulty of breathing in tetraplegics.
METHODS
Study Participants and design
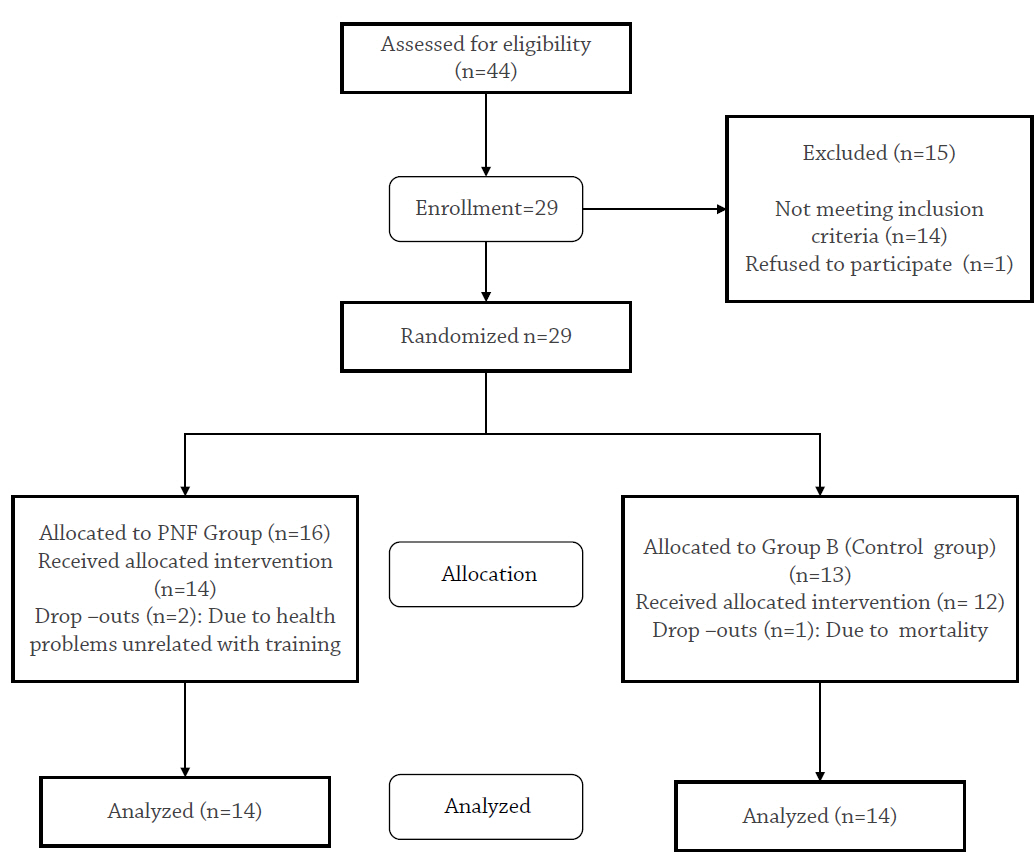
An assessor-blinded randomised controlled trail was undertaken. Purposive sampling was done based on the inclusion and exclusion criteria. The distribution of sample and sample size is explained in CONSORT flowchart (Figure 1). A sample of 29 tetraplegic participants who met the inclusion and exclusion criteria were recruited from Indian Spinal Injury Centre, New Delhi. Tetraplegics (level of injury C5 - C8); ASIA Impairment scale-A and B, 18 - 60 years of age were included in this study. Participants with history of any conditions e.g. periarthritic shoulder, shoulder dislocation, fracture of upper limb and ribs fracture etc. or history of premorbid respiratory conditions (asthma, COPD, restrictive disease of lungs) which may interfere with the training were excluded. This study was approved by research review committee and institutional ethical committee of Indian Spinal Injuries Centre, New Delhi in accordance with the Declaration of Helsinki. A single-blinded, randomized controlled design was undertaken. Participants were randomized to one of two groups using a computer- generated random numbers table. On the first scheduled day of treatment the randomization group was revealed.
The participants were randomly allocated into the following two groups: PNF group - received dupper extremity PNF (with resistance training), CONT group - control group received training with triflow meter. Participants of both the groups underwent their routine physiotherapy exercises.
Procedure for PNF group
A detailed explanation about the treatment protocol was given and participants signed an informed consent. For participants who could not sign the informed consent thumb impressions were taken. Initially, before starting intervention, 1 Repetition Maximum was calculated. Participants were asked to perform PNF patterns D2 flexion – D2 extension with the lowest resistance band (yellow) (Supplementary Materials 1). Resistance was increased till the participants were unable to complete the pattern and then an elastic band of lower resistance was assigned to them for training. The elastic bands started from lowest to highest were yellow, red, green and blue respectively.
For training session, the participants were positioned in side lying on wooden plinth. The one end of the elastic band was tied to the wrist of the extremity that was above and the other end was tied to a wooden block. The therapist stood behind the subject and placed her distal hand on the participants’ hand using lumbrical grip and proximal hand on the radial and ulnar sides of the participants forearm proximal to the wrist. The pattern followed was flexion-abductionexternal rotation with elbow extended and extension –adduction- internal rotation with elbow extended coordinated with breathing, using rhythmic initiation and later progressing to slow reversals. Progression for upper extremity and scapular patterns was given [14]. The training session was given for three sets of ten repetitions, three times a week for a total duration of four weeks.
Procedure for CONT group
Participants were made to sit in an upright position with a triflow type spirometer the mouthpiece connector was held between lips and if required assistance was provided to held spirometer in the vertical position. They were asked to inhale through mouthpiece to lift the 3 balls high as much as possible the spirometer was then inverted and participants were asked to exhale through mouth to lift 3 balls high as much as possible. Training was given for 20 minutes, 3 times per week for a period of 4 weeks.
U tube manometer was used to measure maximum inspiratory pressure (MIP) and maximum expiratory pressure (MEP). For measuring MIP, participants were asked to exhale slowly and completely from the residual volume. A nose clip was attached and participants were instructed to seal lips firmly around the mouthpiece (to prevent air leak) and then pull in hard, as they were trying to suck up a thick milkshake. The largest negative pressure sustained for 1 second on the U tube was recorded. The maneuver was repeated three times with a one minute rest interval after each effort. The highest value recorded was taken for the study. For measuring MEP participants were asked to blow slowly and completely from total lung capacity using the same method as for MIP. Modified Borg scale (MBS) was used to measure the perceived difficulty of breathing. Pre-and post-intervention scores of MIP, MEP and MBS were obtained before and after 4 weeks and data was analyzed.
Statistical Analysis
Statistics were performed using IBM statistical package for social sciences (SPSS) software version 21. Sample size was determined through power calculation based on previous studies with an estimated effect size of 0.80. Analysis was done for 26 participants who completed the study. Independent t test was used for between group analysis, and paired t test was performed for within group analysis between the pre and post intervention scores for both the groups for dependent variables. Level of significance was set at P<0.05.
RESULTS
The PNF group consisted of 14 tetraplegic participants with mean age 30.29 ±13.1 years, duration of injury 3.61± 1.87 months. The CONT group consisted of 12 tetraplegic participants with mean age 25.84±10.57, duration of injury was 3.67±1.83 months (Table 1).
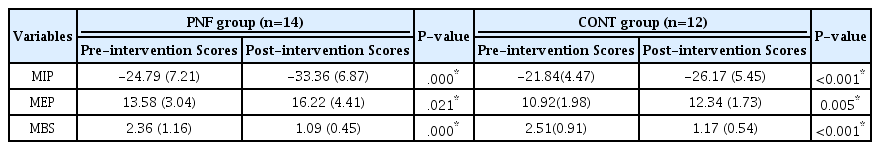
The comparison of pre-intervention scores and post intervention scores of MIP (P=0.001), MEP (P=0.021) and MBS (P=0.001) for PNF group showed significant difference. For the CONT group; the comparison of pre -intervention scores and post- intervention scores of MIP (P<0.001), MEP (P=0.008) and MBS (P=0.001) showed significant difference. The results of within group analysis are summarized in Table 2.
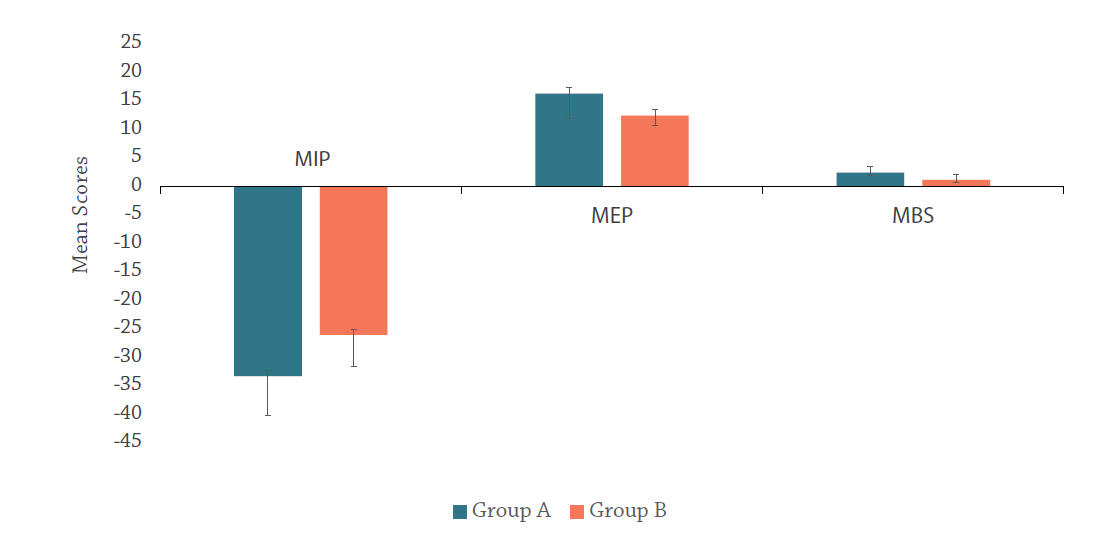
The results of between group analysis are summarized in Figure 2.
DISCUSSION
Respiratory insufficiency due to paresis or paralysis of respiratory muscles is common in tetraplegics. In this study out of 29 participants, 26 participants completed the intervention and 3 participants dropped out from the study. While 2 participants dropped out due to illness, one suffered mortality. We recruited ASIA A and ASIA B only as have no motor innervation below the level of lesion so they were taken in order to remove muscle innervation as a confounding factor to minimize bias. The difference in the pre-intervention scores of MIP, MEP ad MBS of PNF group and CONT group was not significant. Participants with tetraplegia showed a significant improvementin MIP, MEP and scores of MBS. Increased respiratory muscle strength resulted in greater respiratory test values and improved chest wall compliance. The results are in accordance with the findings of previous study [14] on healthy participants in which there was an increase in both MIP (P=0.01) and MEP (P=0.04) after one month of training of upper limb PNF combined with elastic bands.
The probable mechanism for improvement in MIP scores of group receiving PNF (-33.36±6.87) over control group (-26.17±5.45) (P = 0.04 ) can be explained by the principle of irradiation stating that stimulation of strong and preserved muscle groups produces strong activation of injured and weak muscles, facilitating muscle contraction. So, these weak muscles can develop an increase in the duration and/ or intensity by the spread of the response to stimulation [13]. Also, unexercised muscle do become active during resisted upper extremity PNF patterns in normal participants when contralateral limb undergoes an upper extremity PNF pattern [15]. Previous work showed that PNF respiration exercises increases the pulmonary function of normal adults.
There was a significant improvement in MEP scores in PNF group (16.22±4.41) as compared to control group (12.34±1.73) (P=0.04). It was observed that following pectoralis major muscle training there is improvement in muscle strength and expiratory reserved volume [16]. Sternal portion of the pectoralis major is most active in D2 extension pattern of PNF in EMG activities in normal adults [17] and expiratory muscle training leads to an improvement in MEP [18].
The scores of MBS showed a significant improvement in PNF group as compared to control group. It was seen that the effects of levels of perceived difficult in chronic tetraplegics following resistive inspiratory muscle training was decreased [7]. Similar study showed improvement in perceived difficulty of breathing in acute complete cervical spinal cord injury participantss following 6 week resistive inspiratory muscle training [19].
EMG studies can be conducted in the future to understand the pattern of muscle recruitment and follow up can be done to see its long term effects.
CONCLUSIONS
We conclude that upper limb PNF combined with resistance training results in a significant improvement in respiratory muscle strength and rate of perceived difficulty of breathing in tetraplegics as compared to control group.
Notes
Conflict of Interest
The authors declare no conflict of interest.