Influence of Physically Active or Sedentary Lifestyle on Postural Control of Community-dwelling Old Adults
Article information
Abstract
OBJECTIVES
The maintenance of the postural balance is fundamental for the daily living activities, as well as for the practice of physical exercise. However, the aging process and sedentary behavior (i.e., large sitting time) lead to changes biological systems, impairing postural balance with consequent increased falls risk. On the other hand, physical activity practice is a protective factor against these trends. The aim of this study is to investigate the influence of physical activity profile and sedentary behavior on postural control in community-dwelling old adults.
METHODS
This is a cross-sectional study including 208 community-dwelling old adults, which were stratified as sufficiently or insufficiently physically active and with or without sedentary behavior. Then, they were grouped as follow: G1 (sufficiently physically active and without sedentary behavior), G2 (insufficiently physically active, but without sedentary behavior), G3 (sufficiently physically active, but with sedentary behavior), and G4 (insufficiently physically active and with sedentary behavior).
RESULTS
Stabilometric parameters (sway area, total length of center of pressure [CoP] trajectory, and the mean velocity of CP displacement) were obtained to evaluate the postural control. There was significant difference between G1 and G4 on mean velocity of CoP displacement (p < 0.05).
CONCLUSIONS
The coexistence of sedentary behavior and insufficient physically active profile seem to impact negatively on postural control.
INTRODUCTION
Over A physically active lifestyle is understood nowadays as an important factor for the maintenance of health throughout life. In addition to the cardiovascular benefits [1,2], there are also psychological [3], cognitive [4], and musculoskeletal benefits [2,5,6], which is especially relevant for the older adult population.
Conceptually, someone can be classified as physically active based on their living habits if they spend at least 150 minutes per week, or at least 30 minutes a day, with moderate to vigorous intensity activities [7]. Notwithstanding, someone with this profile can simultaneously be classified as having sedentary behavior [8,9], since the remaining time of the day can be dedicated to activities of low energy expenditure ( ≤ 1.5 metabolic equivalent (MET)), such as sitting for reading, watching TV, talking, staying in a lying position, using a computer [10], which justifies the use of "sitting time" as a surrogate term to "sedentary behavior" [11,12].
Differently from the physical activity level classification, which has been well established along several years, the term "sedentary behavior" has been coined in the recent literature, and a cutoff point for hours dedicated to low energy expenditure activities has been investigated [13]. In terms of mortality, specifically in old adults, the study of Pavey et al [14] pointed out the cutoff point of 11 hours / day as significantly associated mortality in the old adults.
Willoughby & Copeland [8] evaluated the effect of a physically active lifestyle in 49 women, 50-67 years old, stratified according to the adoption of sedentary behavior, and the level of physical activity with moderate to vigorous intensity. They investigated cardiovascular outcomes, as well as muscle strength and postural control, however, the analysis was conducted separately for each classification criteria (i.e., physical activety level and sedentary behavior classification). The authors concluded that sedentary behavior was an important risk factor for cardiometabolic disease, whereas a lifestyle with more hours spent with activities with moderate to high intensity seems to be more important for neuromuscular outcomes (ie, muscle strength and postural control).
The approach used by Willoughby & Copeland's [8] is interesting because investigated the physically active lifestyle and sedentary behavior in the same sample, but they make comparison separately (i.e., subjects sufficiently active vs insufficiently active; subjects with vs without sedentary behavior). In addition, they included women who were still young (50-67 years old). At this point it is possible to point out two gaps: 1) How much the interaction between insufficiently physical activity level and sedentary behavior, together, could impact the postural control from old adults? 2) Since aging causes postural control impairment, this analysis in an older population (i.e., ≥ 60 years) may bring new knowledge to the area of postural control.
In fact, as a result of aging process, the sensorial system is impaired (eg, vestibular, visual, proprioceptive), as well as the osteomioarticular system [15], compromising the postural control and consequently the balance, and predisposing the old adults to falls.
Considering the consequences of physical inactivity and sedentary behavior, as well as changes in postural control as a result of the aging process, the present study aimed to evaluate the influence of a physical activity level and sedentary behavior, together, on postural control in old adults.
METHODS
NAll community-dwelling old people (≥ 60 years old) from Aiquara, Bahia, Brazil were invited to take part in this survey study. An extensive health questionnaire, as well as a clinical and physical examination, was conducted in 289 old people that volunteered. Twenty-nine old adults were excluded owing to low score (<13 points) in the Mini Mental State Examination (MMSE), and 52 had technical problems with data collection from variables necessary to meet the proposed aim in this study, then, these 208 older adults comprised the study sample.
The purpose and procedures of the experiment were explained, and consent was obtained prior to the commencement of the experiment. All procedures were approved by the local ethics committee according to the Declaration of Helsinki. Each subject underwent experimental procedures under the same instructions and conditions.
Sample stratification
Volunteers were stratified according to two criteria: the physical activity level and the sedentary behavior. Both criteria were based on answers obtained in the International Physical Activity Questionnaire (IPAQ), adapted for the old adults. The IPAQ adapted for the old adults consists of five domains and fifteen questions regarding physical activity at work, as characteristics of transport, household tasks, recreation and leisure and time spent sitting.
In order to categorize the level of physical activity, the data were dichotomized according to the proposed cutoff point of ≥150 min/week of moderate and vigorous activity (i.e., ≥ 150 min/week, sufficiently active; <150min/week, insufficiently active)[7].
The sedentary behavior was also determined from the IPAQ [16], considering the time (hours / day) spent seated in different places, including at home, in the live group for older adults, doctor's office as well as sitting while resting, watching TV, visiting friends and relatives, reading, making phone calls, and eating. But it does not include sitting time during transportation (e.g., bus or car). The sedentary behavior data were dichotomized according to the cutoff point of 11 hours/day (i.e., ≥ 11 hours/day, with sedentary behavior, <11 hours/day, without sedentary behavior), considering the findings of Pavey et al [14] who observed that this cutoff point is associated with mortality in the old adults.
In order to analyze together the influence of a physically active lifestyle, it was decided to group the old adults into 4 categories:
Group 1 (G1): Old adults sufficiently active and without sedentary behavior (i.e., with a physically adequate lifestyle); Group 2 (G2): Old adults insufficiently active, but without sedentary behavior; Group 3 (G3): Old adults sufficiently active, but with sedentary behavior; Group 4 (G4): Old adults insufficiently active and with sedentary behavior (i.e., with physically inadequate lifestyle).
The characteristics of the old adults from each of the four groups are shown in Table 1.
Stabilometric Measures
Using a piezoelectric force platform (Footwork Pro AM CUBE, France) co-ordinates of the body’s center of pressure (CoP) were recorded during 30s of quiet barefoot standing and sampled at 40 Hz. Volunteers remained with the arms relaxed along the body and were asked to keep the feet parallel, separated at the shoulders’ width, and to look to a target placed at eye level about 2 meter in front of them [17]. The used equipment gives information about the CoP of each foot, allowing measuring the support base width, which was used with height to generate an index “height/support base width” to normalize the body’s CoP displacements, since greater height and smaller support base width trend to increase the amplitude of body’s CoP displacement.
Since diabetes and cataract can influence the postural control of old adults [18], data of the diagnosis of these clinical conditions were obtained from the household survey. Thus, age, diabetes, cataract and “height/support base width” index were used to adjust the parameters stabilometric by applying a mixed model (mixed model) by SPSS software. This procedure aims to adjust the parameters for stabilometric potentially intervening factors.
The body’s CoP displacement was analyzed in MATLAB ® software with previously developed routines to obtain stabilometric parameters: sway area, total length of CoP trajectory, and the mean velocity of CP displacement [19].
Statistical analysis
The studied variables were checked for its normality using the Shapiro-Wilk test. Since the variables age, sway area, total length of CoP trajectory and mean velocity of CoP displacement did not exhibit normal distribution, the between-group comparisons were made using the Kruskall-Wallis test, followed by the Dunn post-hoc test, when necessary. Height and weight were compared with One-way ANOVA, followed by Bonferroni post-hoc test, when necessary. Additionally, the between-group comparisons of categorical variables (sex, diabetes, cataract) were done with the Chi-square test. All statistical procedures were performed in GraphPad Prism v.7.0 software and the significance level was set at p ≤ 0.05.
RESULTS
The sway area, total length of CoP trajectory, and the mean velocity of CP displacement from the studied groups are presented in figures 1-3. Between-group difference (p<0.05) was observed only for the mean velocity of CP displacement (Figure 3). The post-hoc analysis indicated that the mean velocity of CoP displacement was higher in the G4 (insufficiently active and with sedentary behavior) (5.19 ± 0.88 mm/s), when compared to the G1 (sufficiently active and without sedentary behavior) (4.85 ± 0.93 mm/s).
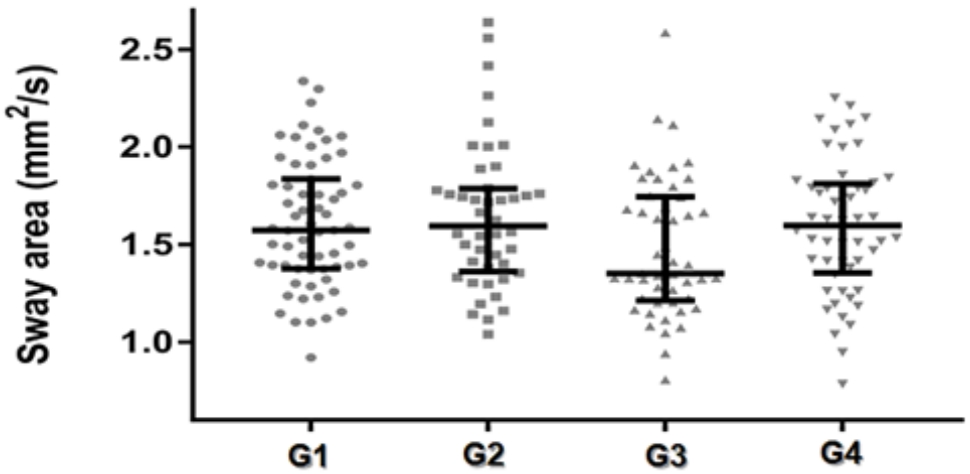
Median ± interquartile range of the sway area of CoP old adults grouped according to the level of physical activity and sedentary behavior.
G1: Old adults sufficiently active and without sedentary behavior; G2: Old adults insufficiently active, but without sedentary behavior; G3: Old adults sufficiently active, but with sedentary behavior; G4: Old adults insufficiently active and with sedentary behavior.
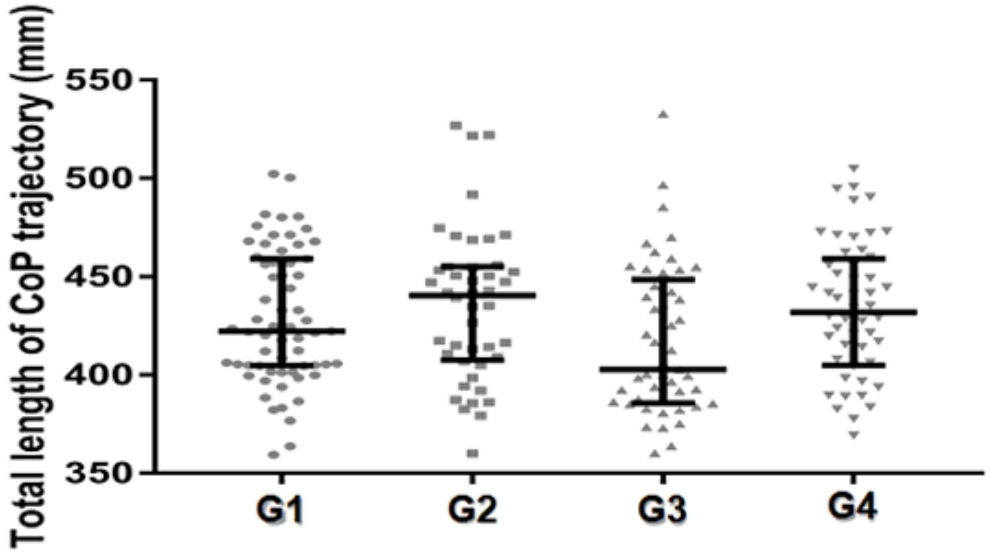
Median ± interquartile range of the total length of CoP trajectory old adults grouped according to the level of physical activity and sedentary behavior.
G1: Old adults sufficiently active and without sedentary behavior; G2: Old adults insufficiently active, but without sedentary behavior; G3: Old adults sufficiently active, but with sedentary behavior; G4: Old adults insufficiently active and with sedentary behavior.
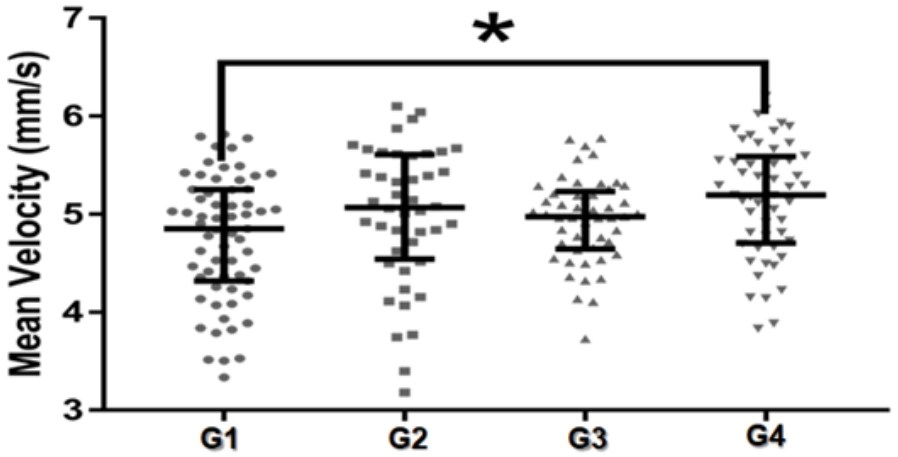
Median ± interquartile range of the mean velocity of CoP displacement old adults grouped according to the level of physical activity and sedentary behavior
G1: Old adults sufficiently active and without sedentary behavior; G2: Old adults insufficiently active, but without sedentary behavior; G3: Old adults sufficiently active, but with sedentary behavior; G4: Old adults insufficiently active and with sedentary behavior. (*) significant difference p < 0.05
DISCUSSION
The present study aimed to evaluate the influence of a physical activity level and sedentary behavior, together, on postural control in old adults. For this, we stratified a sample of old adults into four groups, according to the concepts of physical activity level (sufficiently or insufficiently active) and sedentary behavior (with or without sedentary behavior). Our results demonstrated that a lifestyle with less than 30 minutes per day dedicated to activities of moderate to vigorous intensity and with more than 11 hours per day dedicated to activities of low energy expenditure (especially sitting time) are associated to a pattern of displacement of the CoP with greater speed.
The measurement of the mean velocity of CoP displacement is stated as one of the most reliable stabilometric variables [20], and larger values (i.e., higher velocity of CoP displacement) are associated with aging, in healthy or pathological conditions [21,22]. In addition, the mean velocity of CoP displacement is the most discriminative variable in terms of the evaluation of postural stability changes and age-related risk of falls [23,24,25].
Thus, since the stabilometric data was adjusted for age, our results indicated a worse postural control among the old adults with a lifestyle with less than 30 minutes per day dedicated to activities of moderate to vigorous intensity and with more than 11 hours per day dedicated to activities of low energy expenditure, when compared to old adults with an opposite lifestyle to this one.
It is interesting to note that old adults who were classified as sufficiently active, but with sedentary behavior (G3), as well as those classified without sedentary behavior, but insufficiently active (G2), had intermediate values of mean velocity of CoP displacement, when compared to the two extreme groups (i.e., G1 and G4), allowing to suggest that both criteria may influence postural control, but the adoption of a more adequate lifestyle, as presented by old adults from G1, seems to protect against the decline in postural control.
Indeed, the sedentary behavior does not depend on the individual's moderate to vigorous physical activity level [8,9], and the categorization proposal used here provides a way to analyze the influence of lifestyle on biological variables from older adults.
The used instrument to record physical active lifestyle and sedentary behavior, as well as the transversal design of the present study, are limitations that should be reported. Then, it is suggested that future studies investigate the influence of physical activity profile and sedentary behavior on postural control in community-dwelling old adults using accelerometer to infer physical activity profile and sedentary behavior in a longitudinal study design, aiming to confirm or refute our findings.
CONCLUSIONS
Our results allowed to suggest that old adults with a lifestyle characterized by less than 30 minutes daily dedicated to activities of moderate to vigorous intensity and with more than 11 hours per day dedicated to activities of low energy expenditure exhibit a pattern of CoP displacement with higher velocity, which may represent a pattern of postural adjustment typical of aging and diverse pathological conditions, as well as prone to falls.
Notes
Conflict of Interest
The authors declare no conflict of interest.

