|
 |
| Exerc Med > Volume 7; 2023 > Article |
|
Abstract
OBJECTIVES
The purpose of this study was to compare transversus abdominis muscle thickness and exercise performance before and after foam roller exercise (FRex).
METHODS
This was a randomized controlled trial (RCT). Twenty-four adult female subjects were randomly divided into two groups: (1) an intervention group that underwent FRex, and (2) a control group that remained in the supine position for the same period. Transversus abdominis muscle thickness, modified Star Excursion Balance Test (mSEBT) score, and degree of back pain experienced during daily work were measured before and after the intervention in each group using a visual analog scale (VAS), and a within-group comparison was conducted for each value. The amount of change before and after the intervention was calculated, and the correlation between each measurement item was examined.
RESULTS
Pre-intervention and post-intervention comparisons in the intervention group revealed significantly greater values for transversus abdominis lower fiber thickness and mSEBT scores, and significantly lower values for low back pain after the intervention. A moderate negative correlation was found between changes in lower back pain VAS scores and changes in transversus abdominis lower fiber thickness and mSEBT scores. Moreover, a moderate positive correlation was noted between changes in the transversus abdominis lower fiber thickness and mSEBT scores.
Foam rollers (FR) are used for various purposes including conditioning in sports, rehabilitation in hospitals, and health promotion for the general public. The main purposes of FR are to strengthen core stability (core conditioning) and improve posture [1]. It has various beneficial effects, including expansion of the range of motion (ROM) of the hip joint [2], increase in the ROM of the thorax [1], increase in the flexibility of the hamstring muscles [3], reduction of back pain [3], and alleviation of spinal erector muscle issues [4], as well as subjective effects, such as a lighter feeling (individuals’ comment “I feel lighter”) [3]. Although there are some reports mentioned above, there are insufficient reports on the verification of these effects.
Additionally, the effects of core training have been reported in numerous cases, especially for nonspecific low back pain, and there are reports that core training is effective for improving pain disorders, improving static and dynamic standing balance [5], relieving pain, improving the fatigue tolerance of core muscles, and improving the function of bilateral multifidus muscles in nurses with nonspecific low back pain (NSLBP) [6]. The main purpose of core training is to activate deep trunk muscle contraction and relieve tension in the surrounding large muscles. Among the deep trunk muscles, improving the function of the transversus abdominis is important [7]. The transversus abdominis muscle, together with the deep fibers of the lumbar multifidus muscle, pelvic floor muscle group, and diaphragm, are believed to be involved in increasing the abdominal pressure as a single unit [8]. A delay in the onset of contraction of the transversus abdominis muscle is hypothesized to indicate a defect in motor control and can result in inefficient muscle stabilization of the spine [9]. Furthermore, core stabilization exercises have been reported to improve the rate of change in the transversus abdominis muscle thickness in patients with sub-acute NSLBP [10]. In addition to its effects on lower back pain, Mohamed et al. [11] reported that training of deep trunk muscles, including the transversus abdominis muscle, improved neuromuscular control, which is the ability to control muscle contractions in response to movement and the environment, and significantly improved the findings of the star excursion balance test (SEBT), a measure of dynamic balance.
Various evaluations of deep trunk and core muscles have been reported. Recently, diagnostic ultrasound systems have been used to evaluate the transversus abdominis muscle, and have been shown to have high reliability [12-15]. Based on imaging findings, there are various reports that the thickness and stiffness of the transversus abdominis, thoracolumbar fascia, and multifidus muscles differ between patients with low back pain and healthy subjects [16]. There are also reports on the relationship between improvement in low back pain and changes in transversus abdominis muscle thickness [10,11]. Although evaluating dynamic changes is difficult, it is considered a useful approach for capturing structural changes.
As mentioned above, various effects of core training have been reported; however, few studies have verified the usefulness of techniques involving the use of foam rollers. Hayashi et al. [3] reported the effectiveness of core training for reducing back pain among hospital staff; however, the focus was solely on improving the flexibility of the lower limbs, and the effectiveness of core training as a core training method was unclear. It would be useful to verify whether an improvement in core stability contributes to a reduction in low back pain and trunk stability when considering the adaptation of this exercise approach.
The purpose of this study was to compare changes in transversus abdominis muscle thickness and standing balance before and after foam roller exercise (FRex) in adults with NSLBP and to investigate the usefulness of this exercise for preventing low back pain.
This was a randomized controlled trial (RCT). The subjects were randomly divided into two groups: (1) an intervention group that performed FRex, and (2) a control group that spent the same time in the supine position. The participants were asked about their degree of back pain. Moreover, transversus abdominis muscle thickness was measured, and standing balance was evaluated using the modified Star Excursion Balance Test [mSEBT]). The two groups were compared before and after the intervention twice weekly for three months (Figure 1). The amount of change before and after the intervention was calculated and the correlation between each measurement item was examined.
The participants were randomized using a lottery. To compensate for the disadvantage of no intervention, the same intervention as the control group was conducted after this study with their explanation and consent.
The study was conducted in accordance with the principles of the Declaration of Helsinki. The study’s aim and measurement details (purpose, objectives, and methods) were explained to the subjects orally and in writing in advance, and they were free to decide whether to participate in the study. Measurements were obtained after obtaining written informed consent. For the abdominal ultrasound examinations of female subjects, care was taken to ensure that the measurements were performed by a female examiner in an enclosed and privately protected environment.
The study included 24 adult women (mean age, 24.5 ± 2.71 years) with chronic low back pain. Individuals with specific (disease-named) low back pain and other diseases affecting the measurements were excluded.
Basic information, including sex, age, height, weight, and exercise habits (sports and frequency), was obtained through interviews.
To evaluate usual back pain, the degree of back pain experienced during the past one week was assessed using the visual analog scale (VAS). The average value of the 1-week monitoring was evaluated as the degree of back pain at that time, with 0 indicating “no pain at all” and 100 indicating “too painful to do anything.”
Based on previous studies, the measurement sites were set as follows. The measurement limb was in the supine resting position with the knee joint flexed to 90°. Transversus abdominis muscle thickness was measured before and after the intervention in the supine position on a bed. The measurement site was 2.5 cm medial to the right anterior axillary line on the horizontal line between the upper umbilicus and the floor, and 2.5 cm medial to the superior anterior iliac spine as the middle and lower fibers (Figure 2). During the measurement, the subject was instructed to breathe naturally, such that there was no breath-holding during the task. The probe was placed perpendicular to the measurement site and a static image was recorded after the examiner determined the final stage of expiration, when the subject’s rib cage and anterior abdominal wall were fully lowered. Measurements were performed twice, and the average value was recorded as the measured value. Muscle thickness was measured using an ultrasound system (Konica Minolta, Inc. Sonimage MX1, Tokyo, Japan), and the examination was conducted by the same person who practiced the measurements sufficiently.
The MSEB test was performed to evaluate the dynamic balance by referring to the method described by Hertel et al. [17,18]. The subject stood on one leg, such that the center of the sole of the foot was at the center of a sheet marked every 1 cm on a line extending in three directions (anterior, posterior medial, and posterior lateral) and kept the supporting sole from leaving the sheet. Both hands were placed on the lower back. The subjects were asked to reach as far as possible in three directions from the side of the swinging leg and touch the apex of the foot; the maximum reach distance that could be achieved was measured. The test was invalidated if the subject failed to return to the starting position, if the foot apex left the sheet during the reach, or if the subject used a recoil on the side of the reach. The maximum value was divided by the spinal malleollar distance (the distance from the most prominent part of the superior anterior iliac spine to the most prominent part of the medial phalanx) to obtain the reach rate (%). The reach rate in each direction was summed as the mSEBT score, and the average value of the left and right sides was extracted as the value to be compared for each subject.
The FR used in this study was a stretching cushion PRO (Lindsports Corp., Osaka, Japan; diameter, 15 cm; length, 98 cm; material: polyvinyl chloride cover and an ethylene vinyl acetate copolymer core).
The FRex program, which was performed by the intervention group, was established by referring to programs in the literature [1]. The basic posture in the FR supine position was with both legs hip-width apart and in a relaxed knee flexion position, with the upper limbs in a slightly abducted position and the forearms in an abducted position on the floor. After moving the upper limbs in a circular motion with the back of the hands, a scapular complex exercise was performed with the upper limbs at 90° shoulder flexion and a hip joint internal/external rotation exercise was performed with the hip joint in extension and the heel as the pivot point. The subject again assumed the basic posture, contracted the abdominal muscles in the final range of forced expiration, and performed two sets of exercises to hold the abdominal muscles for 30 s with natural breathing. The following exercises were performed with conscious contraction of the abdominal muscle groups to improve trunk stability: (1) body axis rotation exercises, in which the upper limbs and trunk were rotated slightly to the right and left with both palms in 90° shoulder flexion; (2) upper limb exercises, in which the shoulder joints were flexed 90° alternately on both sides or simultaneously on both sides; and (3) exercises, in which the lower limbs were alternately flexed 90° with one leg off the floor and the hip and knee joints bent to 90°.
Except for the breathing exercises, the exercise program consisted of 10 sessions of 10 min each, and the intervention group continued to perform the exercises twice a week for 3 months. Prior to the intervention, the subjects were presented with photographs of the exercises and the examiner provided verbal explanations of the exercises. We checked and guided the content of the program before the intervention and once a month, for a total of three times.
Since normality was confirmed for all data in the measurement results of this study (Kolmogorov-Smirnov test), p-values and effect sizes (Cohen’s d) were calculated for each group by performing a paired t-test as a within-group comparison of preintervention and postintervention values. For all participants, the amount of change before and after the intervention was calculated for each measurement item, and Pearson’s correlation coefficient test was conducted to calculate the correlation coefficient for each item. The significance level was set at 5% (p value <0.05). All statistical analyses were performed using IBM SPSS Ver. 29 (IBM Corp., Armonk, NY, USA).
Table 1 shows the basic information of the participants. No significant differences were found between the intervention and control groups (Table 1).
Table 2 presents the results of the within-group comparisons. The intervention group showed a significant decrease in lower back pain, a significant increase in transversus abdominis lower fiber thickness, and a significant increase in the mSEBT score, whereas the control group showed no significant differences in any of the items (Table 2).
Table 3 presents the correlation results. A moderate negative correlation was noted between changes in back pain VAS scores, changes in transversus abdominis lower fiber thickness, and mSEBT scores. Moreover, a moderate positive correlation was noted between changes in the transversus abdominis lower fiber thickness and mSEBT scores.
In this study, changes in muscle thickness were compared before and after the intervention in the resting back supine position, and it was found that only the lower fibers significantly increased in thickness after FRex. The transversus abdominis muscle is divided into upper, middle, and lower fibers based on the anatomical differences in the running of the muscle fibers. The middle and lower fibers play important roles in abdominal pressure regulation and anticipatory postural control, with the middle muscle involved in lumbar spine stability via thoracolumbar fascia tension and the lower muscle involved in sacroiliac joint stability [19]. As this study focused on the effect of improving low back pain through the improvement of the stabilizing function of the lumbar spine, we measured the muscle thicknesses of the middle and lower fibers with the expectation that they would change; however, there was a significant increase only in the lower fiber thickness. This indicates that the effect of contraction of the transversus abdominis lower fibers persisted after FRex intervention, and the difference in effect by site was thought to be influenced by the content of FRex implementation. Since pelvic stability is necessary to exercise the lower limbs in an unstable form, it was considered that the lower fibers were more likely to be active for this purpose.
Patients with low back pain have been reported to exhibit a lower transversus abdominis muscle thickness [16]. Moreover, patients with low back pain experience delayed and decreased activity of the transversus abdominis muscle during movement compared to healthy subjects in all directions of limb movement. These findings suggest that reduced transversus abdominis muscle thickness may be a factor in excessive activity of the superficial muscles and the internal and external oblique abdominal muscles, and in low back pain caused by trunk instability. Among the subjects in this study, the transversus abdominis muscle thickness was similar to that reported previously in patients with lower back pain (3–4 mm); however, it is not certain whether it was actually lower because the subjects who did not have lower back pain were not compared in this study. However, exercise therapy focusing on deep trunk muscles was performed for 3 months in patients with chronic low back pain, and the transversus abdominis muscle thickness significantly increased by about 0.4 mm [20], thereby reducing low back pain. In the intervention group of this study, the change in the transversus abdominis lower fiber thickness before and after the intervention was approximately 0.5 mm, suggesting that FRex has a significant effect on increasing activity in the transversus abdominis muscle and may help prevent disability by stabilizing the trunk.
Although there is an association between the transversus abdominis muscle thickness and muscle activity in weak contractions below 20% maximum voluntary contraction (MVC), this association decreases in contractions above 20% MVC, and a low-impact stimulus is considered suitable [21]. In FRex, the transversus abdominis muscle is not forced to undergo strong muscle contractions to ensure core stability of the trunk. Thus, it is thought to be useful as a training approach for this purpose. However, the actual amount of muscle activity on a stretch pole remains a matter of estimation. Therefore, the actual amount of muscle activity when using a foam roller remains a matter of debate. However, FRex is effective in stimulating unconscious contractions. Compared with sitting and standing, which are antigravity positions, this approach is effective from the viewpoint of safety because the patient is kept in the supine position, which is less likely to cause compensatory movements, such as a pain avoidance posture.
The SEBT scores improved after FRex, and the lower limb reach distance increased during standing compared to those in the control group. The transversus abdominis plays an important role in the regulation of abdominal pressure related to thoracolumbar and pelvic stability and anticipatory postural control related to extremity mobility [9]. Moreover, Mohamed et al. [11] showed that deep trunk muscle training improves neuromuscular control and dynamic balance [2]. It has also been reported that FRex increases the ROM of the hip joint, and pelvic girdle stability is thought to contribute to this mechanism. In this study, the increased activity of the transversus abdominis lower fibers may have increased the pelvic stability, including that of the sacroiliac joint and expanded the dynamic stability and mobility of the lower limbs, resulting in improved SEBT scores.
In this study, the effect of FRex on the reduction of low back pain was examined and discussed from the viewpoint of changes in the transversus abdominis muscle thickness. Other factors have also been reported, including left-right differences in erector spinae muscle hardness [4], relaxation of general muscle tension resulting from an expanded ROM of the thorax [1], and improvement of lower limb muscle extensibility [3]. Both muscle thickness and response speed are important [9]. Although the present intervention produced meaningful results in terms of low back pain reduction and improved standing balance, it was not possible to determine which aspects of the intervention were effective in reducing back pain. Although we did not ask the subjects about their subjective impressions or changes in their daily lives, the result that their standing position improved suggests that their daily activities might have also improved, and the positive effects on their back pain might improve their well-being not only at work but also in daily life. Further analyses of other factors should be conducted in the future.
In this study, FRex was the total menu, with all exercises as a set. However, it is important to examine the effects of each exercise in detail, and no previous studies have individually examined the effects of exercises on a foam roller. Therefore, it is important to examine each exercise individually to make it more meaningful. Possible directions for future research are based on the results of this study, such as investigating the long-term effects of FRex and comparing the effectiveness of FRex to other interventions.
The effects of the foam roller exercise on transversus abdominis muscle thickness, standing balance ability, and low back pain were examined in 24 adult female subjects. The results showed significant improvements in lower transversus abdominis muscle thickness, the modified Star Excursion Balance Test, and lower back pain before and after the intervention.
ACKNOWLEDGEMENTS
We would like to express our deepest gratitude to the examinees who cooperated with us in conducting this study.
Supplementary materials
Supplementary materials related to this article can be found at https://doi.org/10.26644/em.2023.002
Fig. 1.
Study Protocol
Abbreviations: VAS, visual analogue scale score; TrA, transversus abdominis muscle; mSEBT, modified star excursion balance test; FRex, form roller exercises.

Fig. 2.
Site of measurement on ultrasound system
1) 2.5 cm medial to the right anterior axillary line on the horizontal line between the upper umbilicus and the floor.
2) 2.5 cm medial to the superior anterior iliac spine Abbreviation: ASIS, anterior superior iliac spine.
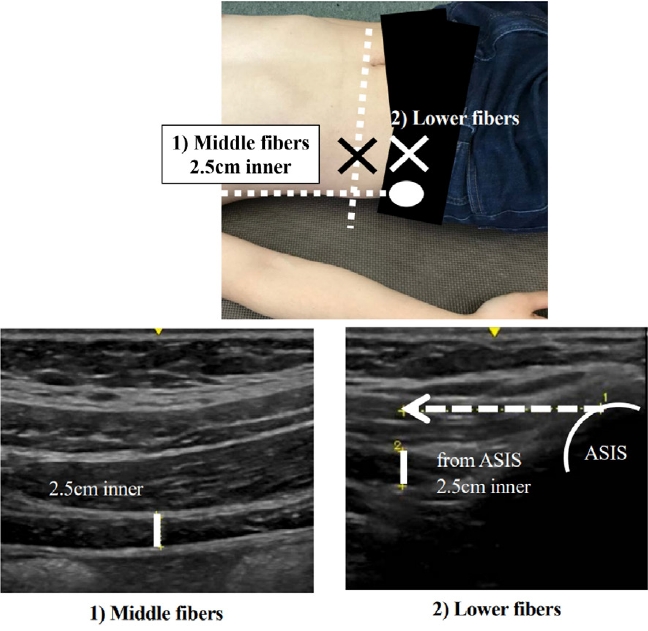
Table 1.
Basic information on the subjects
Table 2.
Results of each evaluation item
|
Intervention group (n = 14) |
Control group (n = 10) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Before | After | p-value | ES | Before | After | p-value | ES |
| Back pain (VAS) | 51.1 ± 20.7 | 32.7 ± 19.6 | 0.03* | 0.91 | 43.3 ± 14.9 | 47.4 ± 19.1 | 0.27 | 0.24 |
| TrA Thickness (mm) | ||||||||
| Middle | 3.0 ± 0.98 | 3.1 ± 0.86 | 0.13 | 0.14 | 3.5 ± 0.82 | 3.5 ± 0.90 | 1.00 | 0.06 |
| Lower | 3.5 ± 0.80 | 4.0 ± 0.74 | 0.01* | 0.63 | 3.9 ± 0.73 | 3.8 ± 0.80 | 0.50 | 0.28 |
| mSEBT (score) | 259.3 ± 13.9 | 272.5 ± 12.6 | <0.001* | 1.00 | 265.7 ± 26.9 | 263.2 ± 24.6 | 0.85 | 0.10 |
REFERENCES
1. Yokoyama S, Gamada K, Sugino S, Sasano R. The effect of “the core conditioning exercises” using the stretch pole on thoracic expansion difference in healthy middle-aged and elderly persons. J Bodyw Mov Ther 2012; 16(3):326–329.


2. Han SW, Lee YS, Lee DJ. The influence of the vibration form roller exercise on the pains in the muscles around the hip joint and the joint performance. J Phys Ther Sci 2017; 29(10):1844–1847.



3. Hayashi M, Matsumoto Y, Ichikawa N, Osada K. Lowback pain alleviation effect of exercising with a stretch pole on the staff members of a long-term care ward. Shimane Journal of Medical Science 2013; 36:73–78. (in Japanese)
4. Yamaguchi K, Kawaguchi K, Sekikawa K, Tabusadani M, Inamizu T. The effect of muscle stiffness and muscle activity in the dorsolumbar region on Stretch Pole® exercise. Journal of Health Sciences, Hiroshima University 2006; 6(1):52–57. (in Japanese)
5. Gorji SM, Mohammadi NSH, Watt P, Henrique MP, Oliveira R. Pain neuroscience education and motor control exercises versus core stability exercises on pain, disability, and balance in women with chronic low back pain. Int J Environ Res Public Health 2022; 19(5):2694



6. Zou CJ, Li JH, Wu FC, Li YZ, Pan HY, Wu T. The effects of core stability training in nurses with nonspecific low back pain. Medicine 2021; 100(25):e26357



7. Teyhen DS, Gill NW, Whittaker JL, Henry SM, Hides JA, Hodges P. Rehabilitative ultrasound imaging of the abdominal muscles. J Orthop Sports Phys Ther 2007; 37(8):450–466.


8. Cresswell AG, Blake PL, Thorstensson A. The effect of an abdominal muscle training program on intra-abdominal pressure. Scand J Rehabil Med 1994; 26(2):79–86.



9. Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine 1996; 21(22):2640–2650.

10. Hlaing SS, Puntumetakul R, Khine EE, Boucaut R. Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain related outcomes in patients with subacute nonspecific low back pain: a randomized controlled trial. BMC Musculoskelet Disord 2021; 22(1):998




11. Mohamed FC, Amer AS, Riziq AG, Khaled AM. Effectiveness of core muscle strengthening for improving and dynamic balance among female patients with patellofemoral pain syndrome. J Phys Ther Sci 2016; 28(5):1518–1523.



12. Kidd AW, Magee S, Richardson CA. Reliability of real-time ultrasound for the assessment of transversus abdominis function. J Gravit Physiol 2002; 9(1):131–132.
13. Bunce SM, Moore AP, Hough AD. M-mode ultrasound: a reliable measure of transversus abdominis thickness? Clin Biomech 2002; 17(4):315–317.

14. Urquhart DM, Hodges PW. Differential activity of regions of transversus abdominis during trunk rotation. Eur Spine J 2005; 14(4):393–400.




15. Koppenhaver SL, Hebert JJ, Fritz JM, Parent EC, Teyhen DS, Magel JS. Reliability of rehabilitative ultrasound imaging of the transversus abdominis and lumbar multifidus muscles. Arch Phys Med Rehabil 2009; 90(1):87–94.


16. Cheung WK, Cheung JPY, Lee WN. Role of Ultrasound in Low Back Pain: A Review. Ultrasound Med Biol 2020; 46(6):1344–1358.


17. Kinzey SJ, Armstrong CW. The reliability of the star-excursion test in assessing dynamic balance. J Orthop Sports Phys Ther 1998; 27(5):356–360.


18. Hertel J, Braham RA, Hale SA, Olmsted-Kramer LC. Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther 2006; 36(3):131–137.


19. Urquhart DM, Barker PJ, Hodges PW, Story IH, Briggs CA. Regional morphology of the transversus abdominis and obliquus internus and externus abdominis muscles. Clin Biomech 2005; 20(3):233–241.

20. Ota M, Kaneoka K, Hangai M, Koizumi K, Muramatsu T. The effectiveness of lumbar stabilization exercise for chronic low back pain-thickness and asymmetry of abdominal muscles. Japanese Journal of Clinical Sports Medicine 2012; 20(1):72–78. (in Japanese)
- TOOLS